| Meningococcus | |
| Pure culture of meningococcus. Gram stain | |
| ICD-10 | G0-G3 |
| ICD-9 | 320-322 |
| DiseasesDB | 22543 |
| MedlinePlus | 000680 |
| eMedicine | med/2613 |
| MeSH | D008581 |
Meningococcal infection
is an acute infectious disease caused by meningococcus, occurring with a variety of clinical manifestations - from asymptomatic carriage and nasopharyngitis to generalized forms (purulent meningitis, meningoencephalitis and meningococcemia with damage to various organs and systems).
Etiology
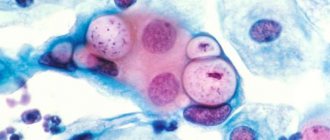
The causative agent is meningococcus - a gram-negative diplococcus Neisseria meningitides. Immobile, has no flagella, does not form spores, aerobic. There is a capsule that protects meningococci from various influences, primarily from phagocytosis. There are several serotypes of meningococcus (A, B, C, D, X, Y, Z, etc.). However, at present, most cases of meningococcal infection are caused by serotypes A, B, C. The main pathogenicity factor is endotoxin. In the environment, meningococcus is unstable and quickly dies outside the human body.
Useful tips
Fortunately, cases of this disease are not common. However, if you learn about the possible spread of infection, you should take preventive measures:
- Do not visit crowded places, especially indoor events;
- If an infection is detected, a thorough examination and subsequent monitoring of children and adults who have been in contact with carriers, the possibility of their admission to children's institutions after negative test results;
- If you come into contact with a sick person, you must undergo a course of preventive treatment with antibiotics and immunoglobulins;
- Mandatory isolation of patients.
It would be a good idea to get vaccinated to protect against possible infection. Vaccination against meningococcal infection is not included in the mandatory calendar, but this vaccine can be used for children from one and a half years of age. It provides immunity for up to five years.
Pathogenesis
The entrance gates are the mucous membranes of the upper respiratory tract (nasopharynx and oropharynx), where the pathogen multiplies. With a high level of local protection and no local changes in the mucous membranes, the person will be a carrier of meningococcus for several weeks. With an insufficient level of local protection, inflammation of the mucous membrane of the nasopharynx develops - nasopharyngitis. In some patients, meningococcus overcomes the local barrier and enters the blood, which can lead either to transient bacteremia without clinical manifestations, or can lead to the development of meningococcemia (meningococcal sepsis). In this case, bacteria are carried through the bloodstream into various organs and tissues: skin, adrenal glands, kidneys, lungs, etc. Meningococcus is able to overcome the blood-brain barrier and cause damage to the meninges and brain matter.
Endotoxin plays an important role in the pathogenesis of generalized forms of meningococcal infection - it is a powerful vascular poison and is released in large quantities when the pathogen dies. By affecting the vascular endothelium, endotoxin causes microcirculatory disorders, which ultimately leads to massive hemorrhages in the internal organs (including the adrenal glands with the development of fatal Waterhouse-Friderichsen syndrome). Edema develops in the brain.
Causes of the disease
The cause of the disease is direct close contact with a sick person or a carrier of the pathogenic bacterium, that is, by airborne droplets. The greatest spread of infection occurs among children, most often under 3 years of age (up to 80%). And it is extremely dangerous for babies in the first year of life, who are most susceptible to developing severe complications. Meningococcus can affect both the central nervous system with the development of purulent meningitis, and other internal organs, causing meningococcal sepsis.
It should be noted that there are many more carriers than patients, and they may look absolutely healthy. The causative agent of the disease lives in the nasopharynx and may not manifest itself in any way. But if there is an inflammatory process in the nasopharynx, then such carriers will be the most contagious.
The main time of illness is winter and autumn. The positive point is that the pathogen dies in the external environment after a maximum of 30 minutes and is very sensitive to its factors, such as temperature, air humidity, etc.
The greatest spread of infection occurs among children, most often under 3 years of age. And it is extremely dangerous for babies in the first year of life, who are most susceptible to developing severe complications.
Clinical classification of meningococcal infection[1]
I. Localized forms:
- carriage of meningococcus;
- meningococcal nasopharyngitis.
II. Generalized forms:
- meningococcemia;
- purulent meningitis;
- purulent meningoencephalitis;
- combined form (meningitis with meningococcemia, etc.).
III. Rare forms:
- arthritis;
- myocarditis;
- pneumonia;
- iridocyclitis, etc.
By severity
:
- Light form.
- Medium-heavy form.
- Severe form.
- Hypertoxic (fulminant) form.
The incubation period (regardless of the form of the disease) ranges from 2 to 10 days.
Types and forms
The most common forms of meningococcal infection are asymptomatic carriage and nasopharyngitis . In the first case, the patient does not know about his infection for a long time.
With meningococcal nasopharyngitis, symptoms may resemble a cold that affects the nasopharynx.
In medical practice, there are two main and one additional groups of meningococcal infection, each of which includes several separate forms of the disease.
Forms of meningococcal infection:
- localized type (asymptomatic carriage of the microbe, meningococcal nasopharyngitis);
- generalized type (meningitis, meningococcal sepsis, combination of meningitis and meningococcal sepsis, meningoencephalitis);
- mixed form (meningococcal arthritis, polyarthritis, pneumonia, endocarditis or iridocyclitis).
The main difference between a localized type of infection and a generalized form is the localization of the pathological process.
In the first case, the disease primarily affects nasopharynx .
In the second case, damage occurs to the circulatory system, brain and central nervous system. The danger of generalized diseases lies in the high risk of death of a small patient.
Clinical manifestations of acute nasopharyngitis
The most common form of meningococcal infection. The disease begins acutely, with an increase in body temperature to 37.5-38.0 °C, accompanied by headache, sore throat, pain when swallowing, and nasal congestion. Lethargy, adynamia, and loss of appetite appear. In the pharynx: hyperemia and swelling of the posterior wall of the pharynx, its granularity - hyperplasia of lymphoid follicles.
Often the disease occurs at normal body temperature, satisfactory general condition and with mild catarrhal symptoms in the pharynx. In the general blood test, there may be a slight neutrophilic leukocytosis, or there may be no changes. The course of meningococcal nasopharyngitis is favorable, recovery occurs on the 5-7th day of illness. However, in some cases, meningococcal nasopharyngitis precedes generalized forms of meningococcal infection.
Features of the disease in children
In children, the course of the disease depends on how weakened the immune system is. But the following features can be highlighted:
- Acute onset of the disease.
- Meningococcal nasopharyngitis in children has symptoms very similar to acute respiratory infections.
- Not all children develop a fever.
- Children get sick more often.
- Rarely are bacteria carriers.
- Clinical manifestations within 5-7 days.
- A runny nose and nasal congestion appear at the very beginning of the disease.
- Nasal discharge contains purulent impurities and mucus.
- There is a possibility that meningococcal infection may develop into generalized forms.
- Changes in blood composition.
- The current is not severe.
- An abrupt onset of the disease and rapid development are possible. In this case, severe symptoms appear, which indicate that the disease is not generalized.
Most often, infection with meningococcal infection occurs in the spring and primarily affects children with weakened immune systems. The child must be constantly monitored, since when the disease passes into a generalized form, the disease develops at lightning speed, and this can lead to death. Therefore, if meningococcal nasopharyngitis is suspected, the child must be hospitalized.
Clinical manifestations of meningococcal sepsis (meningococcemia)
Acute, in many cases, sudden onset of the disease (parents can tell the time of onset of the first symptoms to within an hour) with an increase in body temperature to high values. In addition, there is a headache, refusal to eat, severe malaise, repeated vomiting is possible, and in young children - convulsions. Symptoms increase during the first two days of the disease. At the end of the 1st or beginning of the 2nd day of the disease, a rash appears - first roseola or roseola-papular, of various diameters, disappearing with pressure, located throughout the body. Within a few hours, the first hemorrhagic elements appear: purplish-red in color with a bluish tint, do not disappear when pressed, of various shapes and sizes, rising above the skin. Localized on the lower part of the body: heels, legs, thighs, buttocks. Roseolous-papular elements fade away without a trace after 1-2 days, and hemorrhagic ones become pigmented. Necrosis occurs in the center of the hemorrhagic elements, and where there are extensive hemorrhagic rashes, the necrosis is rejected with the formation of ulcerative defects and scars. In severe cases, gangrene of the fingers, toes, and ears is possible. Rashes in the first hours of illness on the face and upper body are an unfavorable prognostic sign.
Hypertoxic (fulminant) form
meningococcal infection occurs with infectious-toxic shock. The onset is violent with a sudden rise in body temperature to 39.5-40 °C and above, chills, and the appearance of a profuse hemorrhagic rash. The elements of the rash quickly (before our eyes) merge, forming extensive hemorrhages of a purplish-cyanotic color (resembling cadaveric spots). The skin is pale, cold to the touch, and may be covered in sticky sweat. At the beginning of the disease, there is pronounced anxiety in the child, but as shock progresses, the child’s consciousness is depressed until the development of coma. Blood pressure at the onset of the disease is normal, or even elevated, but over time (with further development of shock) it progressively drops, tachycardia occurs, the pulse is threadlike, and shortness of breath is pronounced. All this indicates the development of life-threatening Waterhouse-Friderichsen syndrome. Also, with the fulminant form, convulsions often develop. Body temperature in the terminal stage of shock decreases to normal values, or even low. Among other things, with this form of meningococcal infection, acute swelling and edema of the brain develops. Clinically, this is manifested by severe headache, convulsions, repeated vomiting, and loss of consciousness.
In the absence of proper and prompt medical care, meningococcemia inevitably leads to the development of infectious-toxic shock and death of the patient.
Features of the course and treatment of meningococcal infection in children
February 13, 2014 | No comments | Bacterial infections | Tags: infection
Meningococcal infection is an acute infectious disease caused by meningococcus (Neisseria meningitidis).
It is transmitted by airborne droplets and in its manifestations is characterized by the presence of several clinical forms: meningococcal nasopharyngitis, carriage, meningitis and a generalized form with severe, often fatal changes in the human body.
- 2 Epidemiology
- 3 Pathogenesis
- 4 Classification of meningococcal infection
- 5 Symptoms of meningococcal infection
5.1 Clinic of localized forms: meningococcal nasopharyngitis
- 5.2 Clinic of generalized forms: meningococcemia
- 5.3 Severity of infection
- 5.4 Clinic of generalized forms: meningococcal meningitis
- 5.5 Clinic of generalized forms: meningococcal meningoencephalitis
- 5.6 Clinic of generalized forms: combined form
Etiology
The causative agent of the disease, as mentioned above, is Neisseria meningitides, which appears to be a gram-negative diplococcus. There are 13 serotypes of meningococci in nature. The disease is caused mainly by representatives of serotypes B and C.
Epidemiology
Meningococcus is extremely unstable in the environment. It grows at a temperature of 37C, and already at 35C it cannot reproduce and dies. Moreover, it can remain alive in the mucus from the nasopharynx for up to 2 hours. The microbe dies within 5 minutes at an ambient temperature of +50C. At negative temperatures, death occurs after 2 hours.
The source of infection is bacteria carriers and people sick with this infection. Immunity after illness remains strictly type-specific.
Pathogenesis
When meningococcus enters the mucous membrane of the respiratory tract, an inflammatory process develops, which usually occurs as a result of reduced activity of local immune defense factors. This is how meningococcal nasopharyngitis occurs.
After damage to the mucous membrane, the bacterium enters the bloodstream, causing the manifestation of a generalized form of infection - bacteremia. Purulent meningitis and meningoencephalitis appear when an infectious agent breaks through the blood-brain barrier (BBB). Meningococcus penetrates other organs less frequently.
Classification of meningococcal infection
There are localized forms:
- Carriage of meningococcus;
- Meningococcal nasopharyngitis.
In addition to localized forms, generalized manifestations of infection also occur in the form of:
- meningococcemia;
- meningitis;
- meningoencephalitis.
There are also rare forms:
- arthritis;
- endocarditis;
- iridocyclitis.
Symptoms of meningococcal infection
The period of latent manifestations usually lasts from 1-2 days to 10 days. Most often this period lasts 3-5 days.
Clinic of localized forms: meningococcal nasopharyngitis
At the onset of the disease, body temperature rises sharply to febrile levels. There is difficulty breathing through the nose, and there is practically no discharge from the nose. The pharynx is hyperemic and granular, the arches are swollen and injected. The patient feels a sore throat due to dryness.
Symptoms of intoxication rapidly increase, manifested by headache, loss of appetite, lethargy, and malaise. Improvement occurs after 3-4 days, but after 2-3 weeks the child feels weak and drowsy. In a general blood test, in localized forms, a shift in the leukocyte formula to the left is observed, and the ESR accelerates.
Clinic of generalized forms: meningococcemia
Any generalized form of a disease such as meningococcal infection in children
, may begin with a localized form, that is, nasopharyngitis. As the process generalizes, intoxication increases, fever increases, and a hemorrhagic rash appears.
At the onset of the disease, body temperature rises sharply and suddenly. Parents can name the exact time of onset of the disease in the child. This pathological process is characterized by symptoms of intoxication: headache, nausea, vomiting, which does not bring relief. With meningococcemia, a rash appears.
At first, the rash has a roseolous character, then its elements change and hemorrhagic rashes appear. These elements are dense, do not disappear when pressed, and their diameters are different. Hemorrhage spots tend to merge and form large areas of purple-cyanotic foci. Most often, the rash first appears on the legs and buttocks.
After stopping the process, the roseola elements disappear without a trace, and the hemorrhagic ones go through the stage of pigmentation. If the rashes are large in area, necrosis forms in their central part, trophic ulcers and subsequently cicatricial changes in the skin. If the case of the disease is severe, there is a risk of dry gangrene forming. When a rash appears on the face and eyelids in the early stages, the prognosis of the disease is unfavorable.
Severity of infection
According to the severity of the course, meningococcemia is divided into;
- Light form. Mild meningococcemia is an extremely rare phenomenon. Intoxication is mild, although the temperature rises to 3.5-39C. The duration of fever is only 1-2 days. In the first days, scanty elements of the rash appear on the legs and torso. The rash reorganizes by the 3rd day. Necrosis of the foci does not occur;
- Medium shape. With this form, the condition of the sick child is critically impaired. The body temperature is almost always 40C and a profuse hemorrhagic rash always occurs, which lasts up to a week. Each element has dimensions from 3 to 8 mm. At this time, the patient is inhibited, adynamic, lethargic, and has a sharp headache;
- Severe form. Fever rises above 40C. The rash is localized mainly in the torso and face area. The rash is accompanied by subsequent necrosis, which lasts from 1 to 2 months. With this form, DIC syndrome and shock of infectious-toxic origin often develop;
- Hypertoxic, or fulminant form. This form manifests itself with clinical symptoms of infectious-toxic shock. It occurs quickly and violently with an increase in body temperature to high numbers. Within 4 hours, a completed pathological infectious process with a fatal outcome may develop. If adequate treatment is not started, the patient has no chance of survival.
Clinic of generalized forms: meningococcal meningitis
The onset of the disease is acute with fever and unbearable headache. The child is restless. In the presence of sound stimuli, when turning the head, this symptom intensifies. In this regard, vomiting develops, which can be repeated several times. During the examination of the patient, sharply positive meningeal symptoms of Kernig, Brudzinsky, Lesage, and bulging of the large fontanelle are determined if the child is under one year old. The baby's skin becomes pale.
This condition confirms the presence of meningeal syndrome, the appearance of focal symptoms in the form of nystagmus, and the presence of cerebral symptoms.
Changes typical of meningitis are found in the cerebrospinal fluid: cloudy fluid, neutrophilic pleocytosis, increased protein content, fluid flows out of the needle under pressure.
Clinic of generalized forms: meningococcal meningoencephalitis
Young children are most often affected. The onset of this form of the disease is acute and rapid. As with other forms of meningococcal infection, the temperature rises to febrile levels (38.5-40C). With meningoencephalitis, convulsions and motor agitation may appear. Patients lose consciousness, hemiparesis and damage to the cranial nerves occur. Meningeal syndromes are mild. This form has a high mortality rate.
Clinic of generalized forms: combined form
With this form, the body temperature rises, chills, nausea and vomiting appear.
Meningeal syndrome and the clinical picture of meningococcemia develop.
Meningococcal infection in children of the first year of life
In such babies, the infection most often develops in the form of meningococcemia. And also combined forms. With meningitis, the intoxication syndrome is pronounced. A similarity to meningeal syndrome may also occur in the form of manifestations of anxiety, monotonous screaming (the so-called cerebral scream), bulging and pulsation of the large fontanel, a positive Lesage sign.
Meningeal syndrome appears in full form with a delay of 1-2 days. In infants, the ependyma of the ventricles of the brain, the actual substance of the brain, is often affected, and hydrocephalus develops.
Complications of meningococcal infection
The most common complication is edema-swelling of the brain. In this case, the child’s consciousness is disturbed, convulsions occur and focal symptoms develop, which are unstable, that is, they can disappear and reappear.
The swelling contributes to compression of the brain stem, which leads to coma and increased seizures.
Diagnostics
To detect infection, the main materials for research are nasopharyngeal mucus, cerebrospinal fluid and blood.
Bacteriscopic examination reveals gram-negative diplococci. However, they are visible to the eye only in half of the cases, so the cultural method is widely used.
Meningococcal infection in children and its treatment
Generalized forms of the disease and persons with suspected meningococcal infection should be treated only in an infectious diseases hospital.
Pre-hospital assistance
There are clear algorithms for providing first aid to patients suspected of having this infection and with its obvious presence:
- Administration of chloramphenicol succinate 25-30 mg/kg intramuscularly;
- Prednisolone 2-3 mg/kg intramuscularly. If infectious-toxic shock has developed, it would not be superfluous to administer the entire supply of hormones that is available in the medical bag (10-30 mg/kg);
- Infusion therapy to maintain circulating blood volume (CBV);
- Lytic mixture for suspected meningitis;
- Diuretics - furosemide 1-2 mg/kg;
- Anticonvulsants (diazepam, Relium).
Etiotropic treatment
Meningococcus is still very sensitive to penicillin antibiotics, chloramphenicol, and cephalosporins. If these drugs are ineffective, a reserve group of antimicrobial agents, led by meropenem, is used. Antibiotic therapy lasts from 7 to 10 days.
In parallel with etiotropic treatment, pathogenetic treatment is also used: dehydration, infusion therapy, anticonvulsant, inotropic, plasmapheresis, hemosorption.
- Author: Polina
Hello. My name is Polina. Having once heard the truth that a pediatrician is the main doctor for any family with small children, I realized that I had something to strive for. Rate this article:
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 0 out of 5)
Share with your friends!
Exudative otitis in a child: features of the course and treatment of the disease
Herpesvirus infections and their treatment in children
Clinical manifestations of meningococcal meningitis
Acute onset, with a rise in body temperature to 39-40 °C, severe chills. A severe headache appears (in infants it is expressed as a “brain scream”), without clear localization, children become restless and may clutch their heads. The headache intensifies with any movement, turning the head, touching the head, light and sound stimuli (severe hyperesthesia). Also, with meningitis, there is repeated vomiting, which is not associated with food intake and does not bring relief. Young children often develop seizures. A child with meningococcal meningitis can take a characteristic “pointing dog” position - lying on his side, with his legs bent at the knee joints and his arms bent and brought towards his body. Meningeal symptoms are identified - stiff neck, Kernig's, Brudzinski's, Lessage's symptoms. However, they may be absent or their dissociation may be noted - the presence of some, in the absence of others. The general condition is extremely serious - the pulse is rapid, heart sounds are muffled, blood pressure drops as the disease progresses, and shortness of breath occurs.
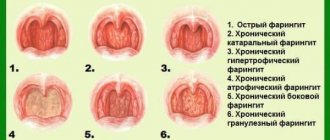
Chronic nasopharyngitis
The chronic form of nasopharyngitis occurs as a result of frequent acute respiratory viral infections and under the influence of predisposing and provoking factors.
I distinguish two main forms of the disease, which transform into one another - hypertrophic and atrophic nasopharyngitis.
Viral agents, bacterial and fungal flora provoke exacerbation of nasopharyngitis in chronic nasopharyngitis.
Provoking factors for the development of pathology are considered:
- structural features and anomalies of the nasopharynx;
- persistent decrease in immunity;
- the presence of foci of chronic infection (sinusitis, caries, pulpitis, adenoiditis, otitis media);
- smoking;
- eating irritating foods;
- occupational hazards or poor environment;
- increased allergization of the body;
- pathology of the digestive system, heart, kidneys, liver.
The hypertrophic form of chronic nasopharyngitis is characterized by a gradual thickening of the mucous and submucosal layer of the nasopharynx, and nasal discharge is often accompanied by lacrimation, often in the morning and the appearance of a large amount of viscous mucus flowing down the back wall of the pharynx.
The appearance of these symptoms requires immediate consultation with an otolaryngologist, clarification of the diagnosis and prescription of comprehensive treatment for the pathology. The price of delay in this case is a gradual transition to the next stage of the disease, which is characterized by irreversible changes in cells and dangerous complications.
With atrophic (subatrophic) nasopharyngitis, the mucous membrane is dehydrated and gradually becomes thinner, and a large number of dry crusts form in the nasal cavity. If left untreated, there is progressive atrophy of the blood vessels and a significant part of the nerve endings of the nose and upper parts of the pharynx.
Laboratory diagnosis of meningococcal infection
The main methods of laboratory diagnosis are: bacteriological and serological studies. The materials for bacteriological examination are nasopharyngeal mucus, blood, and cerebrospinal fluid. In the general blood test: pronounced leukocytosis (in generalized forms), neutrophilic shift towards younger forms, increased ESR.
Cerebrospinal fluid: turbid, flows out in a stream, quickly, due to increased pressure, neutrophilic pleocytosis (usually several thousand cells in 1 μl), a slight increase in protein content, bacteriological examination of the cerebrospinal fluid can reveal meningococci.
Why is it dangerous?
In severe forms of meningococcal infection, the blood supply and metabolic processes in the child’s body are significantly disrupted.
The result of such pathologies can be malfunctions of the liver, kidneys, cardiovascular system, respiratory system and vision. The progression of infection causes inflammation in the joints.
The consequences of meningococcal infection in children can be the following conditions:
- decreased or loss of hearing;
- dry gangrene;
- internal bleeding;
- acute adrenal insufficiency;
- infectious-toxic shock;
- delay in psychomotor development;
- renal failure;
- cerebral edema;
- hydrocephalus;
- pulmonary edema;
- epilepsy;
- pneumonia;
- otitis;
- asthenic syndrome;
- paresis with impaired coordination of movements;
- VSD;
- fatal outcome.
Characteristic symptoms
Meningococcal infection is common in all countries of the world. Most often, the disease is diagnosed in the countries of South America, China and Central Africa. Outbreaks of dangerous infections often occur in countries where residents live in unsanitary conditions.
The causative agent of the disease is the meningococcus Neisseria meningitidis. It belongs to the gram-negative diplococci. Meningococcus enters the human body through airborne droplets. The harmful microorganism affects the oral cavity, nasopharynx, and upper respiratory tract.
The peak incidence of meningococcal infection occurs in the spring months of the year. The disease primarily affects children and people with weakened immune systems.
There are two forms of infection:
- localized (acute meningococcal nasopharyngitis, meningococcal carriage, isolated meningococcal pneumonia);
- generalized (meningococcal meningitis, meningococcal meningoencephalitis)
In some cases, there are practically no symptoms of the disease. With a mild form of meningococcal nasopharyngitis, mild intoxication of the body is observed. The baby usually has a low (subfebrile) temperature. In severe cases, the temperature rises above 38°C.
Children also experience the following symptoms:
- dizziness;
- headache;
- lethargy;
- brokenness.
Meningococcal nasopharyngitis may be accompanied by a sore throat and nasal congestion. The patient often develops mucopurulent discharge from the nasal passages and a dry cough. The skin often looks dry and pale. In severe forms of the disease, the temperature rises above 39°C, and the patient often experiences vomiting and severe headaches.
When examining a patient suffering from nasopharyngitis, swelling of the mucous membrane and redness of the pharynx are revealed. If treatment is started in a timely manner, the duration of the therapeutic course usually does not exceed seven days.
In approximately 30% of cases, the disease meningococcal nasopharyngitis precedes the subsequent development of a generalized form of pathology.
Symptoms and treatment of nasopharyngitis in adults
The greatest risk of developing meningitis and meningococcemia is observed in children. The disease is most severe in children under three years of age. According to statistics, about 75% of patients who died from generalized forms of meningococcal infection are children under two years of age.
In adults, localized forms (healthy asymptomatic carriage of bacteria or nasopharyngitis) are more common. It should be noted that in addition to the presence of favorable facts in the patient that contribute to a more severe course of the disease, some patients also have a genetic predisposition to meningococcal infection.
In such patients there is practically no cellular immune response to meningococci entering the body. In addition to a more severe course of the infection, they also have a tendency to relapse.
In adults living in areas with a large percentage of healthy carriers, specific immunization of the body occurs due to the frequent contact of meningococci on the mucous membrane. Therefore, in groups with a large number of infection carriers, outbreaks of meningococcal nasopharyngitis and meningitis are not recorded.
Symptoms of meningococcal nasopharyngitis in adults do not differ from those in children. Characteristic complaints are weakness, nasal congestion, dryness and sore throat. With light flow, the temperature may not rise. Complaints of hoarseness, dry cough, and scanty viscous discharge from new passages may also be noted.
Due to nonspecific symptoms, meningococcal nasopharyngitis is extremely difficult to diagnose. Meningococcal etiology can be suspected if there is a history of contact between a patient with nasopharyngitis and a patient hospitalized for meningitis.