Viral and bacterial infection: the difference
Viral infection is all diseases caused by a virus.
In order to understand the main differences between viral and bacterial infections, you do not need to be a biologist; it is enough to consider in detail two types of microorganisms: bacteria and viruses. The first are single-celled microorganisms that have an unformed nucleus or no nucleus at all.
Depending on the shape of the cell, bacteria are divided into the following types:
It is worth understanding that throughout life a huge number of bacteria live on the surface and inside the human body. With normal immunity and the general protective state of the body, these microorganisms are not at all dangerous, since they are not pathogens. However, any weakening of the body in combination with other factors will transform innocent bacteria into pathogenic cells that can cause serious illnesses.
Viruses have a negative effect on the cell, so their appearance and activation of development are accompanied by the production of interferon.
The latter begins to interact with other healthy cells and provokes the appearance of an antiviral state. This outcome of events forces the human body to stimulate the immune system and activate hidden protective resources, which are used to fight the emerging disease.
Viruses in most cases live in the human body for a short time, that is, only for the period of illness. However, some of the microorganisms of this class can live in the body all their lives and become active only in certain situations under certain conditions. Such a virus is often not destroyed either by the immune system or by medications (HIV, herpes, etc.).
A general blood test is an effective diagnosis of the presence or absence of infection in the body
A viral or bacterial infection can be determined by a blood test not only by a professional doctor, but also by the patient himself, who has the results of a previously performed diagnostic test.
To determine the source of the disease, it is necessary to carefully analyze each of the indicators presented on the results card. The fact is that, depending on the type of pathogenic cells, some natural changes occur in the structural composition of the blood. By identifying them, you can determine whether you are infected with viruses or bacteria.
So, the general picture of blood test indicators for a viral infection is as follows:
- leukocytes – normal or slightly below normal (very rarely there is a slight increase)
- lymphocytes – above normal
- monocytes – above normal
- neutrophils – below normal
- ESR – normal or slightly increased
Even if all blood test indicators indicate a viral etiology of the disease, it is equally important to analyze the symptoms that appear. The most significant difference between bacterial and viral infections is that the latter has a shorter incubation period (1-5 days).
The development of a bacterial infection in the body also specifically affects the structural composition of the blood
Depending on the type of bacteria that provoke the disease, symptoms and differences in analysis parameters may be slightly different, but in general, a bacterial infection has the following specific features:
- leukocytes - almost always above normal (rarely - normal)
- neutrophils – above normal
- lymphocytes – slightly below normal (less often – normal)
- ESR – increase
- the appearance of young forms - metamyelocytes and myelocytes
As for symptoms, if the disease is bacterial, its incubation period, as a rule, lasts longer than with a viral infection and ranges from 2-14 days.
In any case, even knowing the above features of viral and bacterial infections, determined through a blood test, you should not completely rely on yourself in making a diagnosis. It is important to understand that bacteria are often activated as a consequence of the development of viral microflora, and only a specialist can determine this etiology of the disease.
Diagnosis of viral infection
A general blood test can also show a virus in the blood. But a more detailed picture of a viral infection can be obtained not by a general clinical analysis of the blood substance, but by using the highly informative diagnostic methods of PCR or ELISA.
These two laboratory methods differ from each other in terms of the research mechanism; their only similarity is the high accuracy of the results obtained.
What diagnostic methods for testing blood for viruses are:
- CBC, namely a general blood test, helps to detect the presence of a pathogenic process. With a viral infection, monocytes and lymphocytes will be higher than normal, and leukocytes and neutrophils may also be below the normal limit. The ESR coefficient in this case is normal or slightly increased.
- ELISA, which stands for enzyme immunoassay of blood mass, is intended to identify antibodies or antigens to viruses in the test sample. A viral infection has markers of infection in the form of immunoglobulins IgA, IgM, IgG, produced by the victim’s immune system in response to foreign elements. By analyzing viruses using the ELISA method, it is possible to determine the form of infection: acute, chronic or asymptomatic. Thanks to enzyme immunoassay, it is also possible to monitor the effectiveness of the prescribed therapy.
- PCR, that is, polymerase chain reaction, allows you to determine from the DNA of the virus what type of foreign agent it is. The PCR technique is based on molecular biology because it examines the genetic material of the pathogen. Thanks to this, it is possible to obtain not only confirmation or refutation of the infection and the type of aggressor, but also the number of viruses, as well as their sensitivity to certain medications. Such a detailed clinical picture contributes to making an accurate diagnosis and choosing an effective treatment method. Using polymerase chain reaction, almost all types of viruses and bacteria are detected. The PCR method has a 99% guarantee of reliability.
You can donate blood for a blood test for viral infections at any clinic that has a laboratory, or at a professional diagnostic center. There you can also find out the results of tests for viruses, but it is better if the attending physician deciphers the information received. Because to present a complete clinical picture, symptoms obtained during a survey and examination of the patient are also needed. In addition, auxiliary research methods may be needed, for example, ultrasound, MRI and other instrumental devices.
Useful tips: how to properly treat viral and bacterial infections
Unlike a viral infection, a bacterial one must be treated with antibacterial drugs
As noted earlier, determining whether your infection is viral or bacterial is necessary in order to identify the correct and most effective methods of therapy.
Below are useful tips for treating ailments of these etiological types:
- Returning for the last time to the symptoms of illnesses, we note that a viral infection provokes general physical malaise, fever and a sudden increase in temperature, while a bacterial infection, on the contrary, is activated locally (sore throat, otitis media, etc.), develops for a long time and is accompanied by a low temperature (no more than 38 Co).
- The beginning of therapy for any disease, regardless of its etiological type, should be accompanied by the organization of complete rest and bed rest for the patient. Such conditions should be maintained until almost complete recovery.
- The choice of medications is the most interesting issue in the treatment of viral and bacterial infections. The latter must be treated with antibacterial agents (antibiotics), supplemented with various medications to eliminate local symptoms. Therapy for a viral infection should be accompanied by the use of antiviral drugs and the same drugs aimed at eliminating the symptoms of the disease.
- It is possible to use folk remedies in the treatment of viral and bacterial diseases, but only if it is rational and appropriate.
- Inhalations are also not contraindicated, but it is worth understanding that it is correct to use them only when there are no purulent inflammatory processes in the respiratory tract and the patient has an elevated temperature.
Useful video - How to distinguish a viral infection from a bacterial one:
Only the attending physician can give further advice on the treatment of diseases in a particular case, since it is necessary to take into account the individual characteristics of the disease.
In general, determining a viral or bacterial infection based on the results of a blood test is not a difficult undertaking, requiring only some knowledge. It is important to understand that sometimes your own strength is not enough to organize correct diagnosis and effective treatment, so you should not ignore a visit to the clinic.
Noticed a mistake? Select it and press Ctrl+Enter to let us know.
Acute respiratory viral infections (ARVI) are not uncommon throughout Russia. People call this disease a cold. You can pick it up anywhere, even in summer. In order not to get confused and to know for sure that the causative agent of the disease is a virus or infection, it would be best to donate blood for analysis to make a reliable diagnosis.
How to distinguish a bacterial infection from a viral one, according to numerical data from a blood test
Of course, the main differences in infections of a very different nature are shown by a blood test. When a viral infection occurs, the number of leukocytes remains unchanged, sometimes even decreases.
A change in the normal leukocyte formula is possible if the number of lymphocytes increases or the number of neutrophils decreases. Moreover, the ESR will increase slightly. As an exception, an increase in ESR can also be observed in severe forms of ARVI.
In the presence of a bacterial infection, the white blood cell count increases, resulting from a sharp increase in neutrophils. There is a decrease in lymphocytes, an increase in the number of myelocytes and specific band neutrophils. The patient has a high ESR during this period.
General blood test for ARVI
If you notice cold symptoms, it is important to consult a doctor at the clinic. The purpose of laboratory tests and tests depends on a number of reasons:
- patient's health status;
- types of disease.
Blood is a multifunctional fluid, including a carrier of information about a person’s condition. Therefore, it is her analysis that will be reliable and capacious. The most famous and convenient laboratory test is a complete blood count (CBC), as it has a number of advantages:
- Speed. You can diagnose a liquid in a matter of minutes, which is sometimes very important. But high speed does not mean poor quality. This analysis provides all the basic information about the patient’s condition.
- Unpretentiousness. For such a study, samples can be taken from either a finger or a vein. Which is even a significant plus if a child gets sick. Taking venous blood from him will be a real problem, when it’s much easier to do it out of the blue.
- Price. For people with health insurance, such a study will be free when visiting a clinic. But even if it is not possible to donate blood through insurance, this can be done in any private laboratory at a very affordable price.
The essence of the analysis is that various blood parameters are examined. Depending on gender and age, in the normal state of the body, each indicator should be in a certain range. If he goes beyond the limits, then the person has some kind of pathology. Recently, people who do not have a medical education, using the Internet, can distinguish between basic indicators and learn about ailments based on the results.
Attention! Despite the large amount of information on the Internet, it is best to consult a doctor for a transcript of the analysis.
In case of ARVI, it is important to exclude bacterial infection. This is precisely the main assistant of the UAC. The presence of a virus cannot always be determined by analysis, but bacteria can be identified without problems.
Blood test for children and adults
The onset of the disease has a complex negative effect on the body, and blood is no exception. Due to the disease, its formula changes. UAC allows you to track changes. No special preparation is required for taking it, but it is believed that a blood test taken on an empty stomach will be most reliable. Females are not recommended to donate blood during menstrual periods, and all patients should not take hot baths the day before, eat fatty and spicy foods, or visit saunas and steam baths.
Reference! In addition to the CBC, there is also a clinical blood test (CBC). If the doctor prescribed it, then there is no need to be afraid, since these two tests are essentially the same thing.
The vast majority of people prefer to treat themselves and their children on their own. Because everything seems obvious: runny nose, fever, weakness. There is no point in going to the hospital in this condition. But it won’t hurt to get tested, since the disease may initially be mild, but then complications may appear that could be predicted based on the results of a blood test. In healthy adults, the indicators shown in Table 1 are considered normal.
| № | Index | Norm for men | Norm for women |
| 1 | Red blood cells (RBC),1012/l, tera/liter | 4,4 — 5,0 | 3,8 — 4,5 |
| 2 | Hemoglobin (HBG, Hb), g/l | 130 — 160 | 120 — 140 |
| 3 | Hematocrit (HCT), % | 39 — 49 | 35 — 45 |
| 4 | Color Index (CPU) | 0,8 — 1,0 | |
| 5 | Average value of erythrocyte volume (MCV), fl | 80 — 100 | |
| 6 | Anisocytosis of erythrocytes (RDW), % | 11,5 — 14,5 | |
| 7 | Reticulocytes (RET), % | 0,2 — 1,2 | 2,0 — 12,0 |
| 8 | White blood cells (WBC), 109/l, giga/liter | 4,0 — 9,0 | |
| 9 | Basophils (BASO), % | 0 — 1 | |
| 10 | Lymphocytes (LYM), % | 19 — 37 | |
| 11 | Monocytes (MON), % | 3 — 11 | |
| 12 | Platelets (PLT), 109/l | 180,0 — 320,0 | |
| 13 | Thrombocrit (PCT), % | 0,1 — 0,4 | |
| 14 | ESR, mm/hour | 1 — 10 | 2 -15 |
For children, the normal numbers are those shown in Table 2.
| № | Index | Normal up to a year | Norm |
16 years
In some cases, the standards may differ from those indicated in the table. This depends on the equipment of a particular laboratory. As a rule, most forms with analysis results have a column with the norms for all indicators.
Since ARVI is not one specific illness, but many colds, it is a blood test that will allow us to judge the nature of the course of the disease.
How to understand whether a bacterial or viral infection is based on a general blood test
In the Lab4U online laboratory, we want each of you to be able to take care of your health. To do this, we tell you about health indicators in a simple and clear way!
As a rule, the most common question at the stage of diagnosing a disease that arises from a pediatrician or therapist is whether the patient has a bacterial or viral infection? It turns out that during viral and bacterial infections, two different processes occur in the body. Therefore, the strategy for further treatment depends on the answer to this question.
How is a general blood test done?
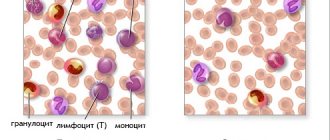
The most informative way to find out the type of infection is to take a general blood test. Human blood consists of plasma and cells of leukocytes, erythrocytes and platelets. The laboratory assistant takes blood from a vein, smears it on a piece of glass, puts it under a microscope and looks at how many leukocytes there are.
They are different: neutrophils, eosinophils, basophils, monocytes and lymphocytes. As a result, he receives a leukogram—the percentage of different types of leukocytes in a stained blood smear under a microscope.
If there are a lot of lymphocytes in the blood, then the disease is viral, and if there are a lot of neutrophils, then the disease is bacterial.
| Test name | Result | Units | Reference values |
| Complete blood count (CBC) | |||
| Hemoglobin | 129 | g/l | 120 – 158 |
| Red blood cells | 4.69 | 1012/l | 3.90 – 5.20 |
| Average red blood cell volume | 82.9 | fl | 81.00 – 100.00 |
| Average hb content in erythrocyte | 27.5 | pg | 26.00 – 34.00 |
| Average hb concentration in erythrocyte | 332 | g/l | 310 – 370 |
| Heterogeneity of erythrocytes by volume | 13.0 | % | 11.9 – 15.5 |
| Hematocrit | 38.9 | % | 34.9 – 44.5 |
| Platelets | 248 | 109/l | 150 – 400 |
| Average platelet volume | 11.7 | fl | 6.0 – 13.0 |
| Heterogeneity of platelets by volume | 15.5 | % | 9.0 – 20.0 |
| Thrombocrit | 0.29 | % | 0.12 – 0.36 |
| Leukocytes | 5.31 | 109/l | 4.00 – 10.50 |
| Leukocyte formula (microscopy) | |||
| Band neutrophils | 6 | % | 1 – 6 |
| Segmented neutrophils | 34 ↓ | % | 41 – 72 |
| Eosinophils | 2 | % | 0 – 6 |
| Basophils | 0 | % | 0 – 1 |
| Monocytes | 9 | % | 4 – 12 |
| Lymphocytes | 49 ↑ | % | 19 – 48 |
Viral infection: there are many lymphocytes, but few neutrophils.
The main cells that neutralize bacteria are neutrophils. The main fighters against bacteria are segmented neutrophil cells. They are often referred to as NS in analysis. It is the most popular cell in the blood.
To become segmented, a full-fledged fighter against bacteria, cells must “mature” and a little time must pass. Initially, a neutrophil in the blood is born as a band neutrophil.
And if the human body begins to fight some microbe, then it begins to actively produce “immature” band neutrophils. Therefore, if there are a lot of these neutrophils in the blood, it means there is an acute bacterial infection in the body.
How and why to distinguish a band neutrophil from a segmented one?
It turns out that this is very easy to do with your eyes, but almost impossible to determine using a machine. That is why it is worth doing not just a general blood test, but a general blood test with microscopy, i.e. with manual examination. Let’s imagine a situation: you or your child have had a fever for the fifth day, you did a general blood test with microscopy.
According to the results, the level of band neutrophils is overestimated. This means that the disease is not viral, but a bacterial complication. And in this case, the pediatrician or therapist understands that it is time to give antibiotics. If you start taking them earlier - when the disease is viral - antibiotics will not only not help fight the infection, but will also weaken the immune system.
This will weaken the body and the risk of bacterial complications will increase several times.
When to take a general blood test with microscopy
Unfortunately, doctors do not always prescribe tests. When making a diagnosis, many people pay attention only to the symptoms: snot, throat, temperature, cough, etc. And this is sometimes fraught with serious consequences.
Our clients often call us and tell us stories related to diagnosis and treatment. And here is one of them. A month ago, Vitaly’s daughter fell ill. She had a high fever and had snot. Attempts to bring down the temperature did not yield results: it remained from +37.5 to +39.
Vitaly turned to the pediatrician. He examined the child and decided to monitor him for four days. On the fifth day there was no improvement, but another symptom appeared - my ears began to hurt. The pediatrician sent Vitaly and his daughter to an otolaryngologist.
At the first examination, the ENT specialist diagnosed the girl with bilateral purulent otitis media. The child was awaiting surgical treatment, a course of antibiotics and physiotherapy.
And all this could have been avoided if Vitaly had taken his daughter to have a general blood test with microscopy before the pediatrician’s appointment, or the pediatrician would have prescribed it at the first appointment. It costs only 310 rubles and is done in one day.
Interpretation of a general (clinical) blood test
For each indicator in a general blood test, there is a range of reference (normal) values. These norms depend on gender and age. Thus, blood test standards for adults and children differ significantly. The interpretation of blood tests in children varies depending on age.
The younger the child, the more his normal blood counts will differ from those of an adult. For example, the number of leukocytes in the first days of a child’s life can be 2-3 times higher than the concentration of these cells in the blood of an adult. And this will not be a deviation from the norm.
| Index | Patient gender | Norm |
| Hemoglobin |
| |
| Red blood cells |
| |
| Leukocytes | – | 4.0-9.0×109/l |
| Hematocrit (the ratio of the volume of plasma and cellular elements of blood) | ||
| Average red blood cell volume | – | 86 – 98 µm3 |
| Leukocyte formula | – | Neutrophils:
Monocytes 3 – 11% Eosinophils 0.5 – 5% Basophils 0 – 1% Lymphocytes 19 – 37% |
| Platelet count | – | 180-320×109/2 |
| Erythrocyte sedimentation rate (ESR) |
Table for deciphering the main indicators of a general blood test.
Deviations from the norm of certain indicators do not indicate the presence of pathological conditions. The results of a blood test can be influenced by severe physical activity on the eve of blood sampling, and in women, also by the phase of the menstrual cycle.
It is known, for example, that the day before the start of menstruation, the level of leukocytes can rise almost 2 times, therefore, the normal values will differ from the standard ones. Therefore, it is better to consult a therapist or pediatrician for interpretation.
If you want to understand for yourself what is happening in the body, you can use the online test interpretation service, where you can enter the indicators of your general blood test and get a preliminary conclusion for free.
Different laboratories may use different units for measuring blood parameters. If they differ from those stated in the online Analysis Decoding service, then you can convert them using a unit conversion calculator.
Conclusions:
To summarize all of the above, a blood test with microscopy can determine what kind of infection (viral or bacterial) we are talking about, how the body reacts to it, and whether it needs the active help of antibiotics. Without the test results during examination, the doctor will not be able to immediately determine the type of infection and prescribe adequate treatment.
If necessary, take a general blood test with microscopy and bring the results to your doctor. This way he can prescribe the right treatment for you.
You can take a general blood test with microscopy with a 50% discount. The analysis will be ready within 1 day. You will receive the results by email as soon as they are ready.
What can be increased or decreased in the blood?
As already mentioned, the presence of a disease in the human body is indicated by deviations in blood test parameters. Since this or that disease on a sheet with test results looks like a set of indicators that go beyond the boundaries of the norm, only a doctor can evaluate the picture in its entirety.
White blood cells are indicators of the functioning of the immune system. If their indicator is too high, then the person’s defense mechanisms are activated, which means there is a pathogen. As a rule, a reaction in the form of an increase in white blood cells occurs to inflammation or allergies. If their number is below normal, then possible reasons include ARVI and infectious diseases such as scarlet fever, rubella and some others.
It is worth noting that leukocytes have the following varieties, which perform different jobs in the immune response.
ESR – erythrocyte sedimentation rate. When studying blood in a laboratory, the rate of sedimentation of fractions is also analyzed. It increases if there is inflammation in the body because the protein content increases. There is no proportional relationship between the disease and ESR, but doctors prefer to take this indicator into account. For example, if at the beginning of the disease it was overestimated, and after treatment was prescribed it began to decline, then the therapy was chosen correctly.
It should be noted that a child can react sharply to a cold and ESR in such cases can be greatly overestimated. In adults, the indicator increases, but not by tens of units. Also, a very increased rate of this speed occurs in acute conditions. In conclusion, I would like to note that the importance of laboratory blood tests in acute respiratory viral infections cannot be underestimated. It is the analysis that allows you to determine the nature of the disease and thereby quickly begin to treat it correctly.
In respiratory viral infection, lymphocytes are often high, but neutrophils and eosinophils are within normal limits. During influenza, lymphocytes and neutrophils decrease, but eosinophils are normal.
Tests for ARVI in children
ARVI, acute respiratory viral diseases, occupy the first place in incidence in children and adults. ARVIs for children are dangerous primarily due to their complications, since they undermine the stability and resistance of the immune system. The formation of chronic foci of infection, allergization, delayed physical and mental development - this is not a complete list of the consequences of ARVI.
ARVI mainly affects children from 6 months to 4 years. This pattern is explained by the fact that in the first half of the year the child has innate immunity, received from the mother, against viruses. Immunoglobulins G (IgG), which penetrated the placenta to the fetus, protect the baby, but gradually their level in the blood decreases. Their concentration in breast milk progressively decreases, and by the sixth month their level is no longer able to meet the needs of the growing baby.
Starting from the age of one, the child’s social circle expands, and the beginning of visiting kindergarten represents a surge of new, hitherto unknown, both impressions and viruses. With each ARVI, the child’s immunity trains to win by releasing antibodies.
The occurrence of ARVI in children is facilitated by the structural features of the upper respiratory tract:
- the larynx, pharynx and trachea are narrow and short, well supplied with blood - there are comfortable conditions for the proliferation of microbes
- chest movements are quite small - conditions for “stagnation” of air with ARVI pathogens
- The rhythm of breathing is not stable - there are no conditions for regular cleaning
The diversity of the viral infection, its variability, speed of spread, and contagiousness make children the first targets for ARVI.
Acute respiratory viral infections, ARVI, are a large and heterogeneous group of infectious diseases of the respiratory tract, which are characterized by symptoms of toxicosis. With ARVI, the mucous membrane of the nose, pharynx, larynx, trachea and bronchi suffers. The mucous membrane of other organs is often affected - the eyes (with adenovirus infection), intestines (with influenza or enterovirus infection), etc.
Among such a huge and motley team of ARVI pathogens, the following are highlighted:
- flu,
- parainfluenza,
- adenovirus infection,
- MS infection,
- rhinovirus infection
since they have their own characteristics in symptoms that are characteristic only of them.
Enteroviruses, herpes viruses and mycoplasma infections can also appear under the guise of ARVI.
Why get tested for ARVI in children?
The purpose of all tests that are performed on a child diagnosed with ARVI is to expose the pathogen. To answer the question - who is guilty?, what will determine the answer - how to treat?
This task is quite difficult, because, as mentioned above, the group of acute respiratory viral infections is heterogeneous and what, in terms of symptoms, is more reminiscent of a banal flu, may turn out to be a herpes infection and vice versa. The number of studies for ARVI can reach 15-20! and the main place here is occupied by determining the level of antibodies to the pathogen.
Runny nose, cough and fever - a triad of main symptoms of ARVI in children
The importance of conducting tests in a child with ARVI is also dictated by the need for immunization - vaccinations. Vaccinations are carried out according to the calendar and deviation from it may negate previous vaccinations. Knowledge of the causative agent of acute respiratory viral infection in a child influences, first of all, the decision about the need for further vaccination against influenza.
There is no need to conduct a large number of tests on a child with ARVI if it is mild and does not cause complications. The most common complication of ARVI is pneumonia.
The following is required: a general blood test at the onset of an acute respiratory viral infection!
A complete blood count is a litmus test that allows you to distinguish a viral infection from a bacterial one. It is almost impossible to distinguish ARVI from a cold by symptoms, only a general blood test with a leukocyte formula. But based on test results, ARVI cannot be distinguished from childhood infectious diseases - measles, rubella, chickenpox.
It should be remembered that the normal result of a blood test in children under 7 years of age is significantly different from that of an adult. When deciphering it, you also need to take into account the general condition of the child, age, previous and hereditary diseases, congenital characteristics, and physiological conditions.
- Red blood cell count is normal or increased due to dehydration
- hematocrit - within normal values, but can increase with significant fluid loss (during fever)
- leukocytes, the most important indicators of a general blood test for ARVI in a child, are at the lower limit of normal or decreased - evidence of the viral nature of the disease
- A general blood test must necessarily contain a leukocyte formula - the percentage of different forms of leukocytes in the blood
- in the leukocyte formula in children with ARVI, lymphocytes predominate, monocytes are slightly increased
- neutrophils decrease during ARVI, and eosinophils may even disappear completely
- if the level of eosinophils increases, the cause of allergization should be looked for - either in the pathogen or in the treatment being carried out (if it has already been started)
- with ARVI in children, ESR is increased;
ESR is a nonspecific indicator of any disease and is unstable, so you should not attach much importance to it. If you have ARVI in a child, you need to take a general blood and urine test
In a general urine test for ARVI in a child, as a rule, no changes are found. Sometimes temporary proteinuria appears - protein in the urine, but the level does not exceed 1 g per day and goes away with recovery.
The appearance of a large number of red blood cells during urine microscopy should alert the doctor to conduct an additional examination of the kidneys. Slight microhematuria is a normal reaction of the kidneys to ARVI.
The results of a biochemical blood test in a child with ARVI are normal if the disease is not complicated.
Immunological studies for ARVI in a child include a range of tests aimed at identifying antibodies to the pathogen. Of interest are exclusively immunoglobulins M, which begin to be released with the onset of the disease. Immunoglobulin G - markers of previous infection does not need to be determined.
The increase in the number of antibodies after ARVI occurs rather slowly. It is necessary to take the test twice - at the beginning of the disease and after 7-10 days. Since most acute respiratory viral infections occur easily and quickly, such a study is simply unnecessary. And yet, it is worth knowing about it, because in some situations, identifying the pathogen is the cornerstone of treatment. Determining antibodies to ARVI pathogens, despite the disadvantages, has a huge advantage - it accurately identifies the pathogen.
In the laboratory diagnosis of ARVI, a general blood test occupies the throne. It must be taken on the first day of illness. A decrease in the number of leukocytes, an increase in the leukocyte count of lymphocytes against the background of a fall in neutrophils are the main features of a blood test in a child with ARVI. General urine analysis and blood biochemistry are usually unchanged. Antibodies are rarely determined in order to accurately identify the pathogen, although the result will be obtained after a double analysis.
pro-analysis.ru
Analysis of urine
Urine is an important product of human life. With it, most toxic substances, breakdown products, hormones, salts and other compounds valuable for research are removed from the body. The percentage of content of a particular substance, the organoleptic and physical properties of the liquid help in the diagnosis of various diseases.
The percentage of urine components varies constantly, as it is influenced by diet, intensity of physical activity, use of medications, dietary supplements, and even emotional state. To avoid mistakes when assessing the patient’s health, prepare the body.
- A couple of days before the test, avoid intense physical activity and bathing.
- Do not drink alcoholic beverages or diuretics.
- During the day, do not eat foods with strong pigmentation (this affects the shade). Such products are: fruits, vegetables and berries of bright colors; smoked, pickled and sweet dishes.
- If you have a disease of an infectious nature, which is accompanied by hyperthermia and increased blood pressure, then postpone taking tests until you have fully recovered, since no conclusion can be drawn based on the results obtained.
- If you have had a cytoscopy, then carry out the tests no earlier than in a week.
- You cannot take the test during menstruation.
If you are taking dietary supplements, vitamin compounds or medications, tell your doctor about this.
Just before taking the liquid, consider the following:
- For analysis, they use the fluid that has accumulated in the bladder overnight, so the collection procedure is performed in the morning, immediately after waking up.
- Wash yourself to avoid foreign particles (including microflora components).
- The collection container must be sterile; use disposable containers.
- To avoid microflora components located on the external genitalia getting into the container, do not lean the container against the skin. For the same reason, release a little liquid, and only then replace the container. 150 ml will be enough for analysis.
- Already collected urine is stored in a closed container for no more than 2 hours at a temperature of 5-8 degrees.
- A special urine bag is used to collect urine from an infant.
When analyzing, experts pay attention to physical, chemical and organoleptic properties, as well as sediment.
Physical properties
In the laboratory, the emphasis is on color, density, odor, acidity and transparency. The color of urine is directly affected by its density, as well as the consumption of brightly colored foods. Normal density ranges from 1003 to 1028 units. In men, urine density is usually higher. The increase in this indicator is also affected by the warm season and dehydration due to diarrhea or vomiting.
The normal acidity level (pH) ranges from 5-7. The change in this indicator is significantly influenced by diet. An increase in this indicator is associated with excessive physical activity, fasting, or excess consumption of fatty foods. The color of urine during normal functioning of the body is warm yellow. Reddish hues indicate pyelonephritis, kidney stones or kidney cancer. Orange – about hepatitis or cirrhosis; black is a sign of alkaptonuria, and pale gray indicates purulent inflammation. Dark urine is often found in ARVI.
Normally, urine has a specific odor, but not a strong one. The smell of ammonia means the presence of inflammation in the genitourinary system, and the smell of acetone means diabetes. The urine of a healthy person does not foam. If foam is present, then conclusions are drawn about heart disease, diabetes or metabolic disorders.
If everything is in order with the body, then the fluid secreted by the kidneys is transparent. Turbidity is a sign of the presence of salts, blood, mucus, pus or bacteria. Depending on what is causing the opacity, a specific pathology is suspected.
Chemical indicators
Normal protein levels range from 0 to 0.033 grams per liter. Exceeding this indicator means the presence of renal pathologies. If the excess is significant and ketone bodies are present in the urine, then diabetes mellitus is suspected. There should be no bilirubin in the urine; if it is present, then the patient has liver problems.
Microscopic examination
Blood cells may be present, but in small quantities. The number of leukocytes should not exceed 5 (low leukocytes in the urine is normal), and erythrocytes - 2. If there are more of the latter, this indicates pathologies of the urinary tract or poisoning. An increase in the number of leukocytes occurs with ARVI, the presence of pyelonephritis, and diseases of the genitourinary system. A healthy person is not characterized by the presence of hyaline, granular or waxy casts; as well as salts, bacteria or fungi.
Based on this text, you cannot diagnose yourself and self-medicate.
A urine test provides valuable information for a specialist and can tell a lot about a person’s physical condition. Follow the rules for taking the test; this will help you get accurate results and avoid mistakes that can cause harm to your health.
In the structure of morbidity, the largest part is occupied by acute respiratory lesions of the respiratory tract and nasopharynx.
In cold weather, the number of colds increases, and in summer it decreases.
If your health deteriorates significantly and recovery does not occur within the expected time frame, there is a need for additional diagnostics. Is it possible to donate blood if you have a cold, and in what cases is it not recommended?
How to determine a viral or bacterial infection using a blood test
- 1 What are viruses and bacteria, what is the difference
- 2 Bacteria are poisonous opportunists
- 3 Viruses are invisible invaders of human cells
- 4 how to defeat cytomegalovirus
- 5 Most common viral infections
- 6, how to determine a viral or bacterial infection using a blood test
- 7 How to determine a bacteria or virus using a general blood test
- 8 Indicators of leukocytes and lymphocytes
- 9, what are the signs of bacterial bronchitis
- 10 Special tests for bacterial infection
- 11 Blood test for procalcitonin - an indicator of bacterial infection
- 12, blood test for HIV, AIDS, tests at home
- 13 Special tests to determine the causative agent of the disease
- 14 DNA - diagnostics, PCR blood test
- 15 Ifa - immunological blood test
- 16, virus, should we panic?
- 17 What is the difference between the treatment of viral and bacterial infections?
- 18 Differences in the prescription of special drugs 18.1 Principles of treatment of viral infections
- 18.2 Treatment of bacterial infections
The causative agents of many diseases are viruses and bacteria. They have many similarities, but there are many more differences. It is very important to know how to distinguish between viral and bacterial infections, since the whole point is in a different approach to their treatment. Blood tests are an effective diagnostic method and help to accurately determine the cause of the disease.
What are viruses and bacteria, what is the difference
To find out how bacteria and viruses affect the body, you need to determine their main differences.
- Bacteria are single-celled organisms
- Viruses have a noncellular structure.
Bacteria are poisonous opportunists
Bacteria are microorganisms that can take different forms:
- circle (“cocci” - pneumococcus, staphylococcus and others);
- oblong bacillus (dysentery and other diseases with a similar clinical picture);
- oval and others are much less common.
- Bacteria, unlike viruses, can develop independently.
- In the human body they find a suitable place for feeding and reproduction.
A myriad of bacteria live inside the human body and on its surface, but if the immune system is functioning normally, they do not pose a danger. However, with the slightest weakening of the immune system, they can cause the development of the disease.
- The bacterium itself does not cause much damage to the body; the toxic products of its vital activity - toxins (exotoxins) - are dangerous.
- The most dangerous exotoxins of all known, which cause diseases such as tetanus, botulism, anthrax, diphtheria, gas gangrene.
- Most bacteria produce toxins as they die and are called endotoxins.
- It is the specific effects of exotoxins and endotoxins on our body that explain the symptoms of each specific disease.
Viruses are invisible invaders of human cells
Viruses are microscopic particles that border between living and nonliving organisms.
- They contain only one type of nucleic acid, DNA or RNA, and exist only inside human cells.
- The host cell processes viral genetic information as if it were its own.
- Viruses do not reproduce on their own; they create copies of themselves at great speed in living cells of the host.
- Thus, in each infected cell there are several thousand of them.
- As a result, the host cells die or become unable to perform their functions, which causes certain symptoms of the disease in a person.
It should be noted that viruses are selective: they capture only those cells that they can force to work for themselves.
- For example, the hepatitis virus can only multiply in liver cells,
- the influenza virus selects the mucous membrane of the bronchi or trachea,
- The encephalitis virus multiplies in brain cells.
- Viruses do not always manifest themselves immediately; sometimes they are activated when the immune system is weakened.
- Some types of viruses (a striking example is HIV) cannot be resisted by the immune system.
The most common viral infections
The most well-known illness is ARVI (acute respiratory viral infection), caused by rhinoviruses, coronaviruses or influenza viruses. The most common diseases include:
- Influenza (flu virus).
- Colds, fever, catarrh or inflammation of the upper respiratory tract (rhinoviruses, coronaviruses).
- Herpes (herpes virus).
- Rubella (rubella virus).
- Measles.
- Poliomyelitis (poliomyelitis).
- Parotitis.
- Viral hepatitis - “jaundice” (hepatitis viruses A, B, C, D, E, F, G and H - we are talking about various viruses that attack the liver, the most common are types A, B and C, of which types B and C may cause liver cancer).
- Papilloma viral infection (warts; some genotypes are also the cause of cervical cancer).
- Rabies (rabies virus, if antiserum is not submitted on time, is 100% fatal).
- AIDS (HIV, human immunodeficiency virus).
- Smallpox (smallpox virus).
- Chickenpox (herpes viruses, type 3 causes shingles).
- Fever, infectious mononucleosis (Epstein-Barr virus, cytomegalovirus).
- Hemorrhagic fever (Ebola, Marburg and others).
- Encephalitis.
- Atypical pneumonia.
- Gastroenteritis.
- Chlamydia.
How to determine a bacteria or virus using a general blood test
The human body reacts to both the bacterium and its toxins in the same way as to viruses, producing antibodies.
- The causative agent of the disease, a bacterial or viral infection, can be determined by the results of blood tests.
- The blood characteristics of a sick and healthy person differ in basic indicators.
- Any deviations from the norm are a consequence of certain disorders in the body. A specialist will easily understand what was the true cause of these deviations.
- A complete blood count can show whether a bacteria or virus is causing the disease.
Indicators of leukocytes and lymphocytes
- One of the main indicators is the level of leukocytes and lymphocytes:
- Leukocytes increase with infection of any etiology.
- But during a bacterial infection, it is neutrophils (this is a special type of leukocyte) that are increased.
- When the number of band neutrophils is increased, they speak of an acute infectious disease.
- But if metamyelocytes or myelocytes are detected, then the patient’s condition is characterized as dangerous and requires urgent medical attention.
- With the help of such diagnostics it is possible to identify the nature and stage of the disease.
- During a viral infection, leukocytes can be elevated, but most often they are lowered (including neutrophils), for example, with influenza, viral hepatitis, measles, rubella, mumps, and typhoid fever, leukocytes are necessarily below normal).
- But with a viral infection, an increase in the number of lymphocytes is necessarily observed, and an increase in monocytes can also be observed (with infectious mononucleosis, for example), so the result of a general blood test is assessed comprehensively.
Bacteriological research
- Bacteriological examination of biological fluid (discharge from the eye, ear, sinuses, wounds or sputum, for example). This test will identify the causative agent of the bacterial infection.
- Analysis of urine.
Shows whether the urinary system is affected by bacteria, and is also necessary to determine the severity of intoxication. - Bacteriological study with antibiogram. Many antibiotics have been developed to fight bacterial infections.
But bacteria also have another unique feature - they mutate, adapting to new conditions and making it difficult to get rid of them.Using this analysis, the type of infectious agent is determined and what medicine can kill it (the so-called sensitivity of the pathogen to antibiotics is determined). These factors are important for prescribing the correct therapy.
Serological study
- Serological study.
Based on the identification of antibodies and antigens that interact in a specific way. For such studies, venous blood is taken. This method is effective when the pathogen cannot be isolated, but the presence of special antigens in the blood will indicate it. - The list of tests is determined by a specialist in accordance with the detected symptoms.
Additional examination
To clarify the result, in some cases, additional examinations are required: X-ray. CT. MRI. Ultrasound or laparoscopy.
Blood test for procalcitonin - an indicator of bacterial infection
It is now possible to distinguish between bacterial and viral infections using a laboratory blood test for procalcitonin levels in order to correctly decide whether to prescribe antibiotics.
The procalcitonin test (PCT) has been used in Western Europe since 2000 and approved in the USA in 2005.
- The concentration of procalcitonin in the blood plasma increases in proportion to the severity of the infectious process, reaching a maximum in the case of sepsis (blood poisoning).
- Since the half-life of procalcitonin (the time it takes for half of the substance to be removed from the blood) is about 25-30 hours and is practically independent of kidney function, its level allows us to monitor the effectiveness of treatment of bacterial infections.
- With proper antibiotic therapy or after successful surgery, the level of procalcitonin in the blood decreases by 30–50% per day. If elevated procalcitonin levels persist for more than 4 days, treatment adjustment is necessary.
DNA - diagnostics, PCR blood test
- A PCR (polymerase chain reaction) blood test allows you to identify diseases in the human body that were caused by viruses or bacterial pathogens.
PCR diagnostics allows you to detect the presence of the following infections in the body:
- HIV;
- Tuberculosis;
- Epstein-Barr virus;
- Toxoplasmosis;
- Listeriosis;
- Shingles;
- Cytomegalovirus;
- Chlamydia;
- Tick-borne encephalitis and many others.
- In addition, hepatitis C can be diagnosed using polymerase chain reaction.
The result of the study is always clear: either negative or positive.
IFA - immunological blood test
- ELISA - Enzyme-linked immunosorbent test (ELISA) is intended for diagnosing infectious, hematological, primary and secondary immunodeficiencies.
—
- The ELISA method has many advantages compared to other diagnostic methods:
- high sensitivity;
- storage stability of ingredients;
- speed of diagnostics;
- a small amount of the test material can be used;
- it is possible to automate all processes;
- infection can be detected at the earliest stages.
Diagnosis, causes of disease, tests
Prescription of correct treatment, its effectiveness and the risk of complications directly depend on timely diagnosis.
- You should consult a doctor at the first alarming symptoms - at the appointment the patient is always prescribed tests.
- Test results help determine a viral or bacterial infection and choose the optimal course of treatment.
- It should be remembered that if the temperature persists for a long time, and the condition worsens after treatment, you need to consult a doctor and conduct additional examination. Since there can be a complication when a bacterial infection joins a viral one and vice versa.
General principles of symptomatic treatment
- Symptomatic treatment is similar for any infection: ensuring complete rest, bed rest and the use of drugs that affect the elimination of the symptoms of the disease.
Principles of treatment of viral infections
Viruses cause a large number of serious infectious diseases.
- There is an effective vaccine against many of them (influenza, hepatitis B)
- against others, drugs that specifically block the viral enzyme were developed (hepatitis C, polio).
- But viral diseases do not have the slightest effect on antibiotic treatment.
Treatment of bacterial infections
Bacteria can cause equally dangerous diseases - bronchitis, pneumonia or even meningitis.
- Therefore, determining the type of causative agent of the disease should be entrusted to a specialist who will not only identify the causative agent of the infection, but also prescribe the optimal treatment method.
- Fighting bacteria with antibiotics is essential to prevent severe disease progression.
- But remember, only a doctor prescribes these medications!
Enzyme immunoassays in diagnostics
How to determine a viral or bacterial infection using a blood test Link to main publication
Source: //analyzekrovi.ru/orvi-orz-ili-gripp/kak-po-analizu-krovi-opredelit-virusnaya-ili-bakterialnaya-infektsiya
Why donate blood if you have a cold?
Tests are considered the main standard of examination in medicine.
- general clinical blood test (CBC), including counting the number of red and white blood cells, platelets, hemoglobin, erythrocyte sedimentation rate;
- detailed analysis with leukocyte formula;
- biochemistry;
- immunogram;
- virological studies using PCR, ELISA;
- bacteriological tests: culture, etc.
The examination allows the doctor to identify the presence of an inflammatory reaction in the body, differentiate a viral process from a bacterial one, and see signs of complications. Using a blood test, you can detect the pathogen, which will allow you to establish the correct diagnosis, assess the degree of the body’s immune response, select treatment and monitor the dynamics of the disease.
Sometimes, under the guise of a cold, serious diseases of an allergic nature, autoimmune and oncological processes begin. A blood test can help identify such conditions. A significant increase in ESR and leukocyte levels, a shift in the formula to the left indicates widespread inflammation. The detection of a large number of eosinophils indicates an allergic reaction.
Blood test indicators
During a general blood test, four indicators are necessarily determined:
- Hemoglobin concentration.
- The number of erythrocytes (red blood cells).
- Leukocyte (white blood cell) count.
- ESR.
A detailed blood test, in addition to the indicated indicators, provides the doctor with information about the average hemoglobin content in a red blood cell, the hematocrit, the number of platelets and the percentage of different types of leukocytes (the so-called leukocyte formula). To differentiate viral and bacterial diseases, the most important indicators are the total number of leukocytes, ESR and leukocyte formula.
Is it possible to donate blood when you have a cold?
A special category of people who donate blood regularly are donors.
In this case, the volume of material taken from one person is much larger than with conventional analysis, ranging from 80 to 450 milliliters.
Since the donor’s blood is intended for another person who is in serious condition, has serious illnesses and often a significant decrease in immunity, it must be carefully examined and safe.
Therefore, if a donor feels the first signs of a cold (headache, malaise, runny nose, sore throat), he is prohibited from donating blood. This is due to the fact that even in the prodromal (initial) period, the virus can be in the blood, and therefore get into the material intended for transfusion to another person.
In addition, the sick person is the source of the pathogen and transmits the disease to others: doctors or other donors, through airborne droplets when coughing or sneezing.
Taking a large amount of blood from a person with an incipient acute respiratory viral infection can worsen his condition and prevent the immune system from fighting the infection.
You are allowed to donate again only a month after you have had a cold.
Most often, blood tests for hormones are paid for. How much does a hormone test cost? Types of examinations and prices are presented in the article.
For an overview of treatment methods for autoimmune thyroiditis, see below.
In what cases and for what indications is it necessary to donate blood for hormones, we will tell you in this article.
Is it possible to do a blood test during a cold?
The volume of standard analysis sufficient to diagnose the disease is small and will not cause any harm to the body.
The attending physician will assess the patient’s condition and prescribe the necessary minimum examination.
Usually you can donate blood either immediately upon application or the next day.
If the test is not related to a cold and was planned in advance in connection with medical examination or other non-emergency medical interventions, then it is better to refrain from donating blood during the period of acute respiratory viral infection. After all, inflammatory changes in the hemogram or changes in biochemical parameters are unlikely to have a positive effect on the course of another disease or will assist in choosing a course of treatment.
It should be remembered that the presence of antibodies in the blood does not always indicate a disease, so it is advisable to carry out immunological tests some time after the disappearance of clinical symptoms. However, standard general tests sometimes have to be repeated during the course of the disease to assess the effectiveness of treatment.
Signs of bacterial infection in a blood test
Pathogenic bacteria settle in tissues and normally do not enter the blood.
Therefore, only those blood cells that are able to leave the bloodstream, penetrate the inflammatory focus and capture the pathogen can fight them. Neutrophils belong to these cells. During acute bacterial infections, the number of neutrophils in the blood increases sharply. Less mature cells appear. This phenomenon is called a shift of the leukocyte formula to the left . The more pronounced the infectious process and the more intense the destruction of mature neutrophils in tissues, the more actively the bone marrow produces and releases band and young cells into the blood. An increase in the number of neutrophils is also reflected in the overall level of leukocytes in the blood - they become much higher than normal - a blood test shows leukocytosis .
During treatment, if it is effective, both the number of leukocytes and the number of neutrophils gradually return to normal. That is, a blood test can serve as a very informative marker of the correct selection of antibiotics. After recovery, the level of white blood cells in the blood remains at the upper limit of normal for some time.
In chronic bacterial infections, moderate leukocytosis and neutrophilia (increased number of neutrophils) are also present, but there is no significant shift in the leukocyte count to the left. If such changes are regularly detected in a person’s blood test and there are symptoms of chronic intoxication (low-grade fever, pallor, weakness, poor appetite), a more detailed examination is indicated. The infection can “sit” in the tonsils, adenoids, kidneys, intestines, respiratory tract, urogenital tract.
As for ESR, in acute inflammatory diseases of bacterial etiology this indicator increases significantly. Its gradual decrease can also be considered an indirect sign of the effectiveness of treatment and a speedy recovery.
Preparing to donate blood
Many people are interested in how to properly donate blood for hormones and other indicators - on an empty stomach or not. It is better to take blood tests early in the morning on an empty stomach. When performing a CBC, capillary blood is collected from the fingertip. A light breakfast is allowed an hour before the procedure, excluding fatty and sweet foods.
It is better to adhere to some restrictions the day before.
The day before the test, it is advisable to drink enough fluid.
But you should give up alcohol. In emergency situations, blood donation is allowed throughout the day, since the benefit from the interpretation of the results obtained is much greater than the possible distortions introduced by non-compliance with the drinking regime or food intake.
Carrying out more complex tests (biochemistry, immunological and other studies) requires taking blood from a vein. Therefore, the training criteria are more stringent. The night before, no more than two hours before bedtime, have a light dinner, excluding fatty, fried, and pickled foods. It is advisable to limit the amount of heavy protein foods and sugars.
Taking alcoholic beverages, soda, and stimulants is excluded. You should also refrain from smoking, since nicotine, when it enters the blood, not only distorts the result, but also causes spasm of peripheral vessels, which makes sampling difficult.
If you can’t give up nicotine, you need to wait at least an hour and only then go and donate blood. The content of some substances in the body at different times of the day may fluctuate, so to get the correct result you need to come for analysis at strictly designated hours (for example, the level of hormones or iron is determined before ten in the morning).
Psycho-emotional and physical stress is also not recommended.
It is better to sit for five to ten minutes before entering the treatment room.
To obtain the most accurate result, you need to know how to properly take hormone tests. Read the patient information sheet.
You can read in detail about the consequences of removing the thyroid gland in women in this material.
It will be necessary to postpone blood sampling if some medical procedures were performed before the study: x-rays, physical procedures. However, in emergency cases, taking blood for analysis is allowed, and the doctor will evaluate the results taking into account possible errors.
A blood test is a medical procedure that helps determine the cause of a cold. It should not be avoided; it does not cause any harm to the body and is carried out as prescribed and under the supervision of the attending physician.
see also
- How to reduce asthma and alt in the blood with medications
- X-ray shop with functional tests
- Urine is cloudy with white flakes in women
- What causes nodules on the thyroid gland?
- How to treat papillomas on the genitals
- What is histology in gynecology
- Why do women have orange urine?
- Signs of leukemia in a blood test in children
- Coagulability according to Sukharev norm
- Fasting blood test for sugar
- Leukocytes in the blood of children, normal table
Video on the topic
| Norm 6 – 12 years | ||||
| 1 | Red blood cells (RBC),1012/l, tera/liter | 3,6 — 4,9 | 3,5 – 4,5 | 3,5 – 4,7 |
| 2 | Hemoglobin (HBG, Hb), g/l | 100 — 140 | 110 — 145 | 116 — 150 |
| 3 | Reticulocytes (RET), ‰ | 3 — 15 | 3 — 12 | |
| 4 | Eosinophils (EO), % | 2 — 7 | 1 — 6 | |
| 5 | Neutrophils (NEUT), % | 15 — 45 | 25 — 60 | 35 — 65 |
| 6 | Reticulocytes (RET), % | 3 — 15 | 3 — 12 | 2 — 12 |
| 7 | Basophils (BASO), % | 0 — 1 | ||
| 8 | Lymphocytes (LYM), % | 38 — 72 | 26 — 60 | 35 — 65 |
| 9 | Monocytes (MON), % | 2 — 12 | 2 — 10 | |
| 10 | Platelets (PLT), 109/l | 180 — 400 | 160 — 380 | |
| 11 | ESR, mm/hour | 2 — 12 | 2 — 10 | |