Left-sided pneumonia is the rarest form of pneumonia, which is recorded much less frequently than right-sided pneumonia, but is a more dangerous form of the disease, which is distinguished by severe clinical symptoms.
If we analyze the entire incidence of pneumonia caused by community-acquired factors, the mortality rate is about 5%. The vast majority of mortality is due to left-sided pneumonia.
The severity of the pathology depends on the type of pathogen, the general immune status of the patient, and the scale of the inflammatory focus. In some cases, pneumonia occurs without characteristic symptoms. A specialized specialist can make a diagnosis based on additional hardware diagnostic methods.
- Antibacterial therapy
How does the disease occur?
The lungs are the main paired organ of the respiratory system, in which oxygen is converted into carbon dioxide. Lung tissue consists of specific cells - alveoli, which perform the main respiratory function.
Anatomically, the left and right lungs are different from each other. The right one is made of three lobes, the left one is made of two, as it has a cardiac notch. Each lobe includes smaller segments.
An inflammatory focus in the alveolar tissue appears after the introduction, fixation and active activity of a pathogenic pathogen - a virus, bacteria, fungus. At the beginning of the disease, the bronchi come under attack, and subsequently the scale of the pathogenic process goes beyond their limits.
The peculiarity of left-sided pneumonia is that pathological transformations of an inflammatory nature can form after injury, surgery, or injections performed in violation of sterility rules. In this case, the infection spreads through the flow of lymphatic fluid or blood.
The descending path of origin of left-sided pneumonia is observed in infective endocarditis. In this condition, bacterial inflammation of the endocardium (the middle lining of the heart) can spread to nearby lung tissue.
Signs of pneumonia, as a rule, are determined only in one lung - left or right. Unilateral inflammation can cover a different area, which determines the form of the disease:
- In a small area there is a focal form.
- In one or more segments - segmental/polysegmental form. In the right lung, segments II, VI, X are most often affected, in the left - VI, VIII, IX, X.
- In a separate lobe there is upper lobe or lower lobe pneumonia.
- In all lobes of the lung there is a lobar form.
If the process spreads to the entire lung, a total form of inflammation is recorded.
Left-sided pneumonia occurs not only when a person is infected by airborne droplets. The source of the disease can be surgical interventions, bacterial infections of internal organs, and endocarditis.
Left-sided segmental pneumonia
Segmental inflammation of the lung tissue is a pathological process that forms in only one segment of the lungs. It differs from the focal type of the disease in that it tends to affect large areas and is more severe than all other types.
A type of problem such as left-sided segmental pneumonia is manifested by acute symptoms and a sharp increase in temperature.
At this moment, the body is completely saturated with toxins, which leads to severe intoxication and severe pain in the chest. Most often, the inflammation takes a protracted course and provokes complications.
If left untreated for a long time, the following complications may occur after the course of left-sided pneumonia of segmental type:
- Fibrous or serous pleurisy;
- Bronchiectasis;
- Chronic pneumonia;
- Neurotoxicosis;
- Collapsed or abscessed lung;
- Arterial hypotension.
Young children and elderly people who have crossed the 50-year threshold are more often infected.
Difference between right-sided and left-sided pneumonia
The formation of left-sided pneumonia is quite rare. This is due to the anatomical properties of the bronchial tree. The fact is that the left bronchus is narrower than the right, which significantly complicates its drainage and blood supply. The peculiar structure negatively affects the completeness of the treatment received. Active drug compounds cannot be transported to the site of inflammation in full. Insufficient drug exposure can significantly delay therapy, contribute to the transformation of the disease into a protracted form, and provoke the development of severe consequences.
Anatomical features allow pathogens of pneumonia to penetrate more easily and quickly into the right lung. The most common pathogens are Haemophilus influenzae, pneumococcus, and staphylococcus. The left lung is most vulnerable to atypical pathogens that infect its cells against a background of weakened immunity.
The formation of inflammation in the upper lobe of the left lung is characterized by its rapid nature, rapid growth and worsening of the clinical picture. Lower lobe left-sided pneumonia is most often recorded in patients with cardiovascular disorders.
Causes of the disease
The disease right-sided pneumonia is due to two possible causes. A person can become infected through airborne droplets or as a result of the activation of bacteria that constantly live in the upper respiratory organs (throat and nose) of a healthy person, if ideal conditions arise for this. The second option is typical in cases of weakened immunity.
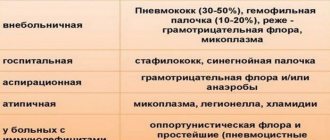
The most common pathogens that cause right-sided pneumonia are:
- streptococcus;
- staphylococcus;
- mycoplasma;
- legionella;
- chlamydia;
- hemophilus influenzae;
- coli;
- fungi and viruses.
Clinical picture
The severity of the disease, the type of pathogen, its susceptibility to specific therapy, the immune status and age of the patient, the scale of the pathological focus - all these are factors that influence the clinical picture of pneumonia.
Community-acquired pneumonia can occur in accordance with two main syndromes:
- Typical syndrome. The disease manifests itself suddenly and is characterized by a sharp increase in body temperature and the appearance of a cough with purulent discharge. Patients complain of pain in the chest. The study identifies areas of compaction in the lung tissue. A typical syndrome develops during infection with aerobic and anaerobic microorganisms, some of which develop in the oral cavity.
- Atypical syndrome. Pneumonia is characterized by a gradual worsening of symptoms. The disease is characterized by the appearance of extrapulmonary symptoms - headache, myalgia, digestive disorders. X-ray shows minor changes in the lung. The disease develops when infected with chlamydia psitaki, tularemia, histoplasma, mycoplasma, legionella, klebsiella.
Signs of the disease depending on the type of pathogen
Symptoms of pneumonia depend on the type of infectious agent. The differences can be clearly presented in the form of a table.
| Pathogen | Features of the clinical picture |
| Mycoplasma | Often leads to hemolytic anemia, erythema multiforme, encephalitis, transverse myelitis, damage to the eardrums |
| Legionella | Characterized by disturbances of consciousness, dysfunction of the liver and kidneys, decreased levels of sodium salts in the urine |
| Chlamydia | Upon examination, wheezing, signs of sore throat, and hoarseness are detected. |
| Staphylococcus aureus | Primary signs are fever and respiratory distress in the form of shortness of breath. Subsequently, sputum joins and the lung tissue thickens |
| Nocardia | The pathology is characterized by the formation of peculiar metastatic foci on the skin and in parts of the central nervous system |
Pneumonia can develop as a complication against the background of an underlying infection:
- During a seasonal outbreak of a specific strain of influenza virus.
- During measles, chickenpox in combination with the appearance of a characteristic rash.
- Syncytial virus is a respiratory infection that is most often seen in children and immunosuppressed adults.
- Cytomegalovirus—in patients with HIV, patients undergoing immunosuppressive therapy after organ transplantation.
If pneumonia is the main pathology, then the clinical picture manifests itself in the form of a rapid increase in body temperature, fever, and a persistent dry cough without sputum production. The addition of extrapulmonary symptoms is typical. Against the background of measles, flu or chickenpox, respiratory dysfunction occurs, which provokes the development of secondary pneumonia.
Pneumonia of secondary origin can form simultaneously with the main infectious disease, regardless of its viral or bacteriological origin. In some cases, pneumonia manifests itself as a long-term complication, several days after the main symptoms have subsided.
Complications after pneumonia in children
In childhood, they develop very quickly; treatment should be started as soon as possible. Complications can occur during illness and during periods of weakening. In children, infectious-toxic shock occurs, which is provoked by endotoxins of viruses or microbes. In this case, the temperature rises, the pressure decreases, and a characteristic rash appears. Coma may occur.
A common form of complications is pulmonary failure. Breathing becomes rapid and shallow, shortness of breath appears, the lips and nasolabial triangle acquire a bluish tint.
One of the severe complications of pneumonia in children is pulmonary destruction, when lung tissue is destroyed. Cardiopulmonary failure can lead to death.
Main symptoms
Clinical manifestations are not much different from pneumonia of other localizations. Patients complain of:
- Significant increase in temperature up to 40°C.
- Boring cough.
- Attacks of night sweats.
- Sticky sputum.
Upon examination, tachypnea, cyanosis of the nails, and acrocyanosis are determined.
The same form of pneumonia occurs completely differently in different patients. Verification of the same pathogen cannot mean the same course of the disease and a similar prognosis in different patients.
Symptoms of the disease
Inflammation of the left lung, in terms of symptoms, completely coincides with other localizations of the disease. And here it is important to identify the disease as quickly as possible and begin its treatment:
- heat;
- coughing;
- weakness throughout the body;
- sweating at night;
- expectoration of sputum when coughing in large quantities;
- blue lips and nails;
- rapid breathing;
- incipient fever.
Bacterial and viral pneumonia are very different. With viral inflammation, a person is plagued by weakness, headache, fever and dry mouth, as well as a severe cough. Bacterial pneumonia is characterized by fever and sputum production when coughing.
Left-sided pneumonia in a child is especially severe. In the very early stages of the disease, the child may experience a high temperature of up to 40 degrees and a severe dry cough. At the same time, severe shortness of breath may occur, which manifests itself not only during physical activity and while the child is at rest. The baby may complain of severe chest pain and hiccups.
Exactly the same symptoms will be observed in older people. The symptoms will not be as severe. After 60 years of age, pneumonia can lead to loss of spatial orientation and frequent fainting.
Diagnostics
The doctor may notice the first signs of left-sided pneumonia when examining the patient. During breathing movements, the lag of the left part of the chest is visually determined. When percussing over the affected areas of the left lung, a shorter sound is recorded. Auscultation reveals fine bubbling rales and signs of crepitus.
The final diagnosis is made after an X-ray examination. The images show areas of infiltration in the upper or lower lobe. If more detailed, clarifying information is required, computed tomography and bronchoscopy are indicated.
Laboratory diagnostics. To establish the type of pathogen, a bacteriological analysis of sputum is performed.
A blood test allows you to establish the level of leukocytosis with a shift in the formula, a higher ESR. Blood biochemistry determines the parameters of the main plasma protein.
Consequences
After suffering from pneumonia, a number of changes in the bronchopulmonary or other systems, such as adhesions, scars and others, may be noticeable.
Bacteremia
With insufficient antibacterial therapy, bacteremia may develop, that is, the circulation of microorganisms in the bloodstream. This condition is very dangerous, since the microbes in the blood have a toxic effect on vital organs - the brain and heart. With prolonged exposure, the function of the latter is impaired, leading to death. To identify this complication, blood taken from a vein is used, which is sown on nutrient media. If bacteria grow on them, it means that human blood contains microorganisms. Massive doses of antibacterial drugs are used for treatment.
Endocarditis
Due to the close contact of the lungs and heart, both anatomically and functionally, the consequences of diseases of the former can negatively affect the cardiovascular system. Thus, the infectious process can migrate through the bloodstream to the heart, causing an inflammatory process there.
In this case, the inner lining of the heart, the endocardium, is most often affected, and the disease is called endocarditis. Since the valves are derived from the inner membrane, they are subject to severe changes in this pathology - adhesions may appear in them, which will disrupt blood circulation.
Pleurisy
Each lung is enveloped in a connective tissue membrane, the pleura, and the chest cavity is also lined with it. Between these two leaves there is a slit-like space containing a minimal amount of liquid. This structural feature of the lungs allows them to carry out movements in the chest when breathing.
In the absence of treatment or insufficient antibiotic therapy, as well as the location of the source of inflammation too close to the pleura, the process can spread to it, as a result of which pleurisy develops. In this condition, adhesions may occur between the sheets or excess fluid may accumulate. In both cases, this limits the motor activity of the chest organs, breathing becomes more difficult and requires serious therapeutic measures.
In the first case, treatment is carried out for massive adhesions and mainly surgically separate them; in the second, the cavity between the pleural layers is punctured and the accumulated fluid is released.
Respiratory failure
As noted above, the development of the inflammatory process entails blocking the exchange of gases in the alveoli. When large volumes of lung tissue are affected, the oxygen enrichment of the blood is significantly reduced. This condition in which the lungs cannot fully meet the body's oxygen needs is called respiratory failure. In this case, the oxygen-dependent nervous system, in particular the brain, is greatly affected.
With such a complication, a person needs quick and intensive medical care. To save life, the patient is connected to a ventilator, which maintains the concentration of blood gases at an optimal level.
Scar changes
The development of inflammatory phenomena in any organ entails the proliferation of connective tissue, which forms adhesions or scars. At the height of the disease, this mechanism is protective in nature, as it limits the focus from other parts.
Such scars also form in the lung tissue. As a rule, they do not lead to serious consequences and appear only on X-ray images in the form of dark spots. However, in rare cases, they can be the cause of a persistent cough. Treatment in this case does not cause difficulties and is carried out with drugs that promote resorption.
Abscess
In some cases, long-term pneumonia can lead to the formation of an abscess, which is a limited accumulation of pus. When listening, hard breathing disappears, however, the patient continues to complain that it is also difficult to breathe and the temperature persists. A rounded spot of darkening will be visible on the x-ray.
As such an abscess develops, it can open into the bronchus or the above-mentioned space between the layers of the pleura. The first option is more favorable since its contents are released when coughing, breathing becomes easier, adhesions form in the cavity and the patient’s condition improves. In the second case, the outcome is less rosy, as the purulent contents accumulate and cannot be released, which requires urgent puncture or surgical intervention.
Treatment
As we have said many times, left-sided pneumonia requires long-term complex treatment.
Doctors are faced with a number of tasks:
- Elimination of the infectious agent.
- Restoring the drainage function of the bronchi.
- Stabilization of general immunity and resistance of the lungs to external factors.
Antibacterial therapy
Antibiotics are prescribed as early as possible, at the slightest suspicion of pneumonia. This step allows you to alleviate the main symptoms and prevent the development of complications. The prescription of a particular drug is carried out by a doctor. He also determines the duration of antibiotic use.
If pneumonia resolves without exacerbation of other chronic disorders in a mild or moderate form, drugs of the aminopenicillin and macrolide class are prescribed. In cases where pneumonia is aggravated by concomitant pathologies, it is advisable to use cephalosporins of the II-III generation, amoxiclav in combination with macrolides of the latest generation.
If the patient’s condition does not improve within 2-3 days, the antibacterial drug is changed. A certain positive effect is observed when prescribing fluoroquinolones of the III-IV generation (moxifloxacin, levofloxacin). If pneumonia goes away without complications, treatment at home is allowed. The patient takes all prescribed pharmaceuticals, and the attending physician periodically visits him and monitors the dynamics of the disease. When a person notices positive results from therapy, one should not stop taking a particular drug on their own. This can aggravate the overall picture of the disease, especially in infants, children, and older patients. Only a doctor prescribes or cancels treatment.
Severe pneumonia requires hospitalization of the patient in a specialized department. Antibacterial drugs are administered intramuscularly or intravenously. First, aminopenicillins are prescribed. If treatment does not produce positive changes, the use of the latest cephalosporins, macrolides, and respiratory fluoroquinolones is started.
Pulmonary and extrapulmonary complications
As a rule, pneumonia is successfully treated and goes away without complications. But for some high-risk patients it can be dangerous. Complications may be related to mild or medications used. In addition, pneumonia leads to exacerbation of chronic diseases such as obstructive pulmonary disease (emphysema) or congestive heart failure.
Complications of pneumonia include:
- pleurisy;
- septicemia and (or) bacteremia (blood poisoning);
- pulmonary abscess;
- heart problems;
- apnea or respiratory failure.
A rather unpleasant consequence of the disease can be diarrhea and a fleeting rash, which are side effects of some medications used.
Pleurisy
Inflammation of the pleura, the two thin balls between the lungs and chest, occurs in both children and adults. Less commonly, fluid may accumulate in this space (exudative pleurisy). About half of patients hospitalized with pneumonia suffer from exudate.
The fluid puts pressure on the lungs, making breathing difficult. The body usually copes with pleural effusion as the disease is treated.
In one out of ten cases, the exudate that caused pleurisy becomes infected with bacteria. This provokes the accumulation of pus (pleural empyema). The infected fluid is removed using a thin needle. In the most serious cases, surgery is required to remove pus and damage to the pleura and lungs.
Lung abscess
Pulmonary abscess is a fairly rare complication after pneumonia. Mainly observed in people with severe chronic illnesses who are dependent on alcohol. With an abscess, cavities filled with pus develop in the lungs.
Symptoms of an abscess in patients are:
- unpleasant smell of sputum;
- swelling of the toes and hands.
Treatment of an abscess involves intravenous antibiotics at the beginning of therapy, then you should take tablets for another 4-6 weeks
It is important to complete the recommended course of antibacterial drugs, even if the patient feels better, to prevent re-infection
Bacteremia and blood sepsis
Bacteremia is a condition in a patient's body in which bacteria have entered the bloodstream. Delayed diagnosis leads to the accumulation of bacterial toxins in the blood. This signals the immune system to produce cytokines, which cause inflammation. This creates a serious, complex body response known as blood poisoning (septicemia).
Symptoms of sepsis in pneumonia:
- High temperature (above 38°C).
- Fast heartbeat and rapid breathing.
- Low blood pressure (hypotension), causing dizziness.
- Mental behavior disorder (disorientation).
- Decreased diuresis.
- Pale, moist skin.
- Loss of consciousness.
Due to blood poisoning, the infection can affect other organs and systems of the body, causing meningitis, peritonitis, septic arthritis or endocarditis. Treatment of metastatic infections requires high doses of intravenous antibiotics.
Modern methods of treatment of left-sided pneumonia of the lower lobe localization
The doctor can prescribe effective treatment only after carrying out diagnostic measures, during which he will establish the final diagnosis of “left-sided lower lobe pneumonia” and identify the causative agent of this inflammatory process. The pathogen is identified by analyzing expectorated sputum, which takes some time. While waiting for the results of this analysis, treatment of the patient is still prescribed according to the generally accepted scheme - medications with a high content of broad-spectrum antibiotics. As soon as the causative bacteria is identified, the attending physician will immediately prescribe narrow antibiotics.
As already noted, this type of pneumonia must be treated in a hospital setting. It is under these conditions that doctors will be able to guarantee their patients a complete recovery.
To treat left-sided lower lobe pneumonia, a qualified doctor will prescribe second and third generation antibiotics:
- Levofloxacin is an antibacterial drug that belongs to the group of third-generation fluoroquinolones (intended to suppress DNA synthesis and for profound morphological changes in bacteria - cytoplasm, cell wall, membrane).
- Cephalosporin is an antibiotic based on 7-ACC (damages the cell walls of bacteria that are at the reproduction stage, leading to their death due to the release of autolytic enzymes).
- Amoxicillin is a semi-synthetic antibiotic that has a wide range of effects on aerobic gram-positive bacteria, aerobic gram-negative bacteria and microorganisms.
- Sulfamethoxazole is a combination antimicrobial drug used not only for its treatment, but also for prevention.
- Azithromycin is a semi-synthetic antibiotic that belongs to the azalide subclass (its action is aimed at slowing down the growth of bacteria and their reproduction).
The attending physician monitors the effectiveness of the prescribed antibiotic treatment during the first two to three days. If there is no improvement in the patient's condition, then another drug is prescribed. In case of a positive effect from the prescribed medications, the course of treatment is carried out for two weeks.
In addition to antibiotics, the doctor prescribes medications to his patient:
- to dilate the bronchi so that phlegm is better removed;
- to thin sputum;
- to boost the immune system.
The use of traditional medicine is also encouraged.
Diagnosis of pneumonia
If the described symptoms occur, it is necessary to contact a specialist as soon as possible in order to diagnose and prescribe appropriate treatment. There are several ways to diagnose right-sided pneumonia:
- radiography of the right lung to determine the size and location of the focus or lesions of the disease (right-sided upper lobe pneumonia, left-sided, lower lobe, etc.);
- sputum analysis;
- blood test for leukocyte levels;
- bronchoscopy to examine the bronchi and possible collection of mucous contents.
Only a specialist can establish a diagnosis and prescribe treatment in the case of pneumonia and only with the help of the necessary tests, so you should not independently diagnose such a serious disease. It is better to consult a doctor in time.