During the period of exacerbation of colds and flu, many people are faced with various kinds of pathological conditions. These include a frontal sinus cyst, the existence of which you may not even suspect. It is formed due to the fact that the secretion secreted by the glands ceases to be excreted and accumulates, bursting the sinuses from the inside.
Typically, this neoplasm is discovered after diagnosing the respiratory system if other diseases are suspected. To do this, the patient undergoes an X-ray examination and the tumor can be seen in the image. Symptoms and treatment of cysts depend on the individual.
general information
A frontal cyst forms in the frontal sinuses due to the effects of mechanical processes, inflammation, trauma, and weakened immunity. Quite often, the pathology is diagnosed in patients with chronic frontal sinusitis. The neoplasm is distinguished by the presence of a dense wall with a mucous membrane and liquid inside. It can form without infection or with infection by various microorganisms.
The method of treatment is determined by the attending physician after diagnosis. Depending on individual characteristics, drug or surgical treatment is chosen. The operation is prescribed only after passing certain tests and a thorough examination.
Treatment of a cyst in the frontal sinus
If the symptoms of the disease are pronounced, and the development of complications is observed (or suspected), surgical treatment is indicated for patients. However, in the early stages of pathology, it is possible to use conservative techniques. Currently, drug treatment of frontal sinus cysts is aimed at achieving the following clinical results:
- Liquefaction of the secretory clot.
- Provoking reflex opening of the anastomosis of the frontal sinuses.
- Escalation of contents from the paranasal frontal sinuses.
- Restoration of tissue immunity.
- Restoration of aeration of the frontal sinuses.
- Removing swelling and washing the cavity of the frontal sinuses.
Thanks to the use of medications to eliminate edematous-inflammatory processes, otolaryngologists are able to achieve stable opening of the anastomosis of the frontal sinuses. After this, various tanning substances are introduced into the sinus cavity, which wash the cyst and promote its resorption.
Sometimes, with cystic pathology, spontaneous emptying of the frontal sinus through the nose can be observed. It should be remembered that such a mechanism for removing pathological contents from the frontal sinus does not lead to clinical recovery. As the disease progresses, the cyst will again fill with mucous, purulent or serous contents.
Subsequent conservative treatment is aimed at reducing the hypertrophied mucous membrane. Thanks to this, it is possible to eliminate cyst symptoms such as impaired nasal respiration, as well as headaches and local pain. In the absence of positive results from therapeutic treatment, patients suffering from frontal sinus cysts are indicated for surgical intervention.
Diagnostics
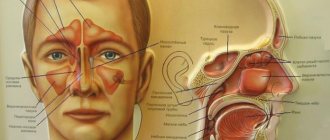
Diagnosis of a frontal sinus cyst occurs in the following ways:
- An x-ray from two angles allows you to see dark spots in the area of formation. If the cavity is not completely filled with fluid, it is extremely difficult to see the neoplasms;
- CT diagnostics shows high accuracy. To determine the size, depth and exact location, CT is complemented by MRI;
- use of an endoscopic instrument with a camera. It is inserted into the nasal cavity;
- probing and puncture of fluid from the nasal cavity allows you to determine the presence of a cystic formation.
After diagnosing and making an accurate diagnosis, the doctor can choose the most effective method of treatment.
Symptoms
Symptoms of a cyst can be noticed as it grows and develops. Typically, at the acute stage of the disease, the following symptoms are noted:
- dizziness, loss of consciousness;
- headache that gets worse during bending or physical activity;
- pain in the area of the tumor, radiating to the eyes;
- structural changes, drying of the nasal canals and mucous membranes;
- breathing becomes difficult;
- purulent discharge.
During the examination, the doctor may feel a new growth of a hard, round shape, similar in consistency to plasticine. Manifestations of the cyst are noted in the form of bulging of the eye, as the neoplasm begins to put pressure on it. Signs of a cyst in this case manifest themselves in the form of profuse lacrimation, blurred vision, and dysfunction of the lacrimal canal.
If you ignore the tumor, it may soon burst, its contents will come out and can penetrate the brain, triggering the development of meningitis and other inflammations. In advanced forms, drug treatment does not show good results, so the patient is prescribed surgical methods.
Frontal sinus cyst: symptoms, treatment, surgery, how to remove it
A frontal (or frontal) sinus cyst is a benign tumor that usually occurs due to obstruction of the excretory ducts. As a result of the accumulation of mucus, the patient experiences difficulty breathing, headache, and loss of consciousness.
The patient experiences difficulty breathing, headache, and loss of consciousness.
Development mechanism
The lower region in the frontal sinus is covered with epithelial tissues. The glands produce a secretion that provides moisture to the space.
This mechanism delays pathogenic microorganisms and protects against infectious diseases. The liquid contents pass through the epithelium, but sometimes clog the existing passages.
Mucus accumulates in the tissues, causing a cavity to form on the right or left side.
Due to accumulated mucus, a cavity forms in the right or left side.
Gradually, the secretion accumulates, and the seal increases in size, blocking the nasal passages.
The peculiarities of a frontal sinus cyst include the fact that it does not degenerate into a malignant tumor. This type of tumor only rarely resolves with the use of medications.
It is often detected in children and adolescents or in older people.
Symptoms of a frontal sinus cyst
It is not possible to immediately determine the presence of a benign tumor in the sinus. As it grows, the patient will notice the following signs:
- the nose will be constantly stuffy, making it harder to breathe. The condition will worsen during sleep;
- pain will appear in the frontal part of the head, which will be stronger under any load.
We are talking about flights, bends and other situations that involve a strong change in the usual body position or pressure; Pain in the frontal part of the head. - while moving the eyes, the patient will feel excessive tension;
- Diseases in the nasal sinus will worsen more often, and there will be copious secretion of mucus and pus;
- the person will experience loss of smell.
As the cyst grows in size, additional symptoms will appear. The seal will protrude in the part of the forehead where it is localized. Pressing on the lump hurts.
In the future, unpleasant sensations can spread to the jaw, eye socket, and gums. The eyeballs can and will bulge forward. If the capsule spontaneously ruptures, a viscous secretion flows through the nose. Subsequently, visual disturbances and constant lacrimation develop.
Complications
If the cyst is not treated or the wrong method is chosen, the patient develops serious complications. Due to active growth, the formation compresses the eyeball, displacing it downward, and exophthalmos develops. The patient experiences double vision and vision becomes worse.
An enlarged tumor causes a fistula. The purulent contents of the cyst can penetrate into the orbit and cranial cavity. This leads to severe inflammatory processes in nearby tissues. Complications caused by cystic formation cannot be treated with medication. To eliminate them, surgical therapy is prescribed. Typically, treatment requires removing all damaged tissue.
Causes
Atheroma or sebaceous gland cyst on the face is a benign neoplasm that develops as a result of blockage of the sebaceous duct. The pathology is popularly called “wen.” Most often, tumors are localized in places where a large number of glands accumulate: on the forehead, wings of the nose, chin, cheeks, temples. Sometimes pathology develops on the upper eyelid or scalp. The main causes of the disease are considered to be:
- environmental pollution negatively affecting air quality;
- summer period, when hot weather provokes intense production of sebum or sebum;
- professional activities associated with prolonged stay in a dusty room;
- use of low quality cosmetics;
- incorrect or incomplete removal of decorative cosmetics from the skin of the face;
- violation of the rules of facial hygiene, provoking the proliferation of pathogenic microorganisms on the skin;
- oily skin type, tendency to form acne, oily seborrhea, regular occurrence of acne, pimples;
- hereditary predisposition;
- increased work of the sweat glands, promoting the proliferation of pathogenic microbes;
- failure of metabolic processes;
- weakened immunity as a result of frequent colds, deficiency of vitamins in the diet;
- hormonal imbalance causes atheroma to appear on the forehead and other areas, especially in women.
In men, a predisposing factor to the appearance of a cyst on the cheek can be irregular shaving or grooming of the beard. In addition, there are pathologies that provoke the production of large amounts of testosterone, which affects the condition of the epidermis. Long-term use of potent medications can also cause illness, as it weakens the immune system and reduces the body's resistance to bacteria and viruses.
Treatment methods
Frontal sinus cysts are treated in several ways. Surgical therapy is prescribed in late forms of the disease, since drug treatment is no longer effective. To decide on the type of treatment, you need to undergo a full examination and tests.
Without surgery
Conservative treatment is effective only in the initial stages of pathology development. The complex of drug therapy includes:
- Sinupret – has pronounced anti-inflammatory properties. The plant base promotes the rapid outflow of fluid from the frontal sinuses, reducing the risk of complications;
- Amoxicillin (semi-synthetic antibiotic) is used to eliminate the infection;
- Bioparox spray copes with inflammation of the mucous membrane. The product also shows good results in the fight against infections;
- Naphthyzin is prescribed to eliminate edema;
- mucolytic agents are used to liquefy accumulated secretions;
- physiotherapy (warming, washing the sinuses) is the basis of conservative treatment.
To enhance drug therapy, you can resort to traditional medicine methods. Before using any traditional recipes, it is important to consult with your doctor. Otherwise, there is a possibility of complications. Typically used to treat nasal canals:
- radish juice drops;
- inhalations with chamomile, eucalyptus and lemon balm;
- washing with solutions of medicinal herbs;
- warming up the sinuses with hot sand, table salt, and a hard-boiled egg.
Cyst in the frontal sinus: symptoms and treatment
A cyst in the frontal sinus is a pathological cavity that develops in the frontal bone, behind the brow ridges.
A benign neoplasm can have different contents - sterile secretion, serous fluid, purulent impurities. In the vast majority of cases, the cause of the appearance of a cyst is a violation of the outflow of mucus secreted by the sinus membrane. The cyst may not manifest itself for several years, which often makes it difficult to find the reasons for its development. Diagnosis requires additional research - an annual examination by an otolaryngologist is not enough. Treatment of cysts is always surgical; the complexity of the intervention and the prognosis after surgery depend on the presence of complications.
Causes
A cyst of the frontal sinus (frontal sinus) is a spherical cavity with thin, stretched walls. There are 3 types of fluid that can fill a cyst :
- sterile secretion of the mucous membrane of the sinuses - characteristic of a mucocele cyst;
- purulent contents – pyocele;
- serous fluid - hydrocele.
In rare cases, a cyst develops that is filled with air, stretching the sinuses (pneumosinus) or thinning the bony walls of the sinuses (pneumocele).
All of the listed neoplasms (except for pneumocele) are of a retention nature. Such cysts are called true cysts - they contain an internal lining of epithelial cells. The mechanism of their development is as follows:
- Blocking of the nasal duct, through which the secretion of the mucous membrane of the frontal sinus exits into the nasal cavity (normally, mucus is necessary to moisturize the nasal passages and protect against inhaled pathogenic flora, toxic and allergic agents).
- The production of secretion continues, it accumulates in the sinus, it is supplemented by decay products - ventilation and the composition of the sinus environment are disrupted.
- Accumulated toxins irritate the sinus mucosa, causing an increase in the volume of mucus produced and its further accumulation.
- The mucous and bony walls of the sinus cannot withstand the pressure, they become thinner with the formation of cracks through which the secretion escapes into neighboring areas, deforming them.
The growth process of a tumor in the frontal sinus can be triggered by:
- Domestic, sports and other injuries to the nasal mucosa or skull bones - years can pass from the moment of injury to the onset of symptoms, so the patient often does not even connect these events.
- Overlapping of the frontonasal canal with bone growths, often with osteoma (benign bone tumor).
- Chronic inflammation of the nasal cavity or paranasal sinuses - directly the frontal sinuses (frontitis), nasal passages (rhinitis), maxillary sinuses (sinusitis), larynx (laryngitis), pharynx (pharyngitis). This is also true for allergic inflammations and frequent acute inflammations.
- Adhesions and scar growths resulting from sinusitis of the frontal sinus.
- Degenerative changes in the inner lining of the frontal sinuses.
- Polyps in the nasal cavity.
- Infectious diseases affecting the respiratory tract - scleroma or syphilis.
- congenital anatomical features - a thin frontonasal canal, a displaced hard palate or nasal septum - we are not talking about a congenital cyst, but about the presence of a factor contributing to its appearance.
A pyocele (cyst with purulent contents) can:
- develop due to infection of a mucocele;
- become the result of a latent infectious process in the frontal sinus, which is not completely controlled by the selected dose of antibiotics.
The reason for the development of pneumocele is the appearance along the frontonasal canal of a kind of “valve” (capable of blocking the air flow) - it can be a polyp, an edematous area or a post-traumatic scar.
In rare cases, congenital cysts may be found in the frontal sinus , which appear as a result of intrauterine development disorders.
Symptomatic manifestations
A small cystic “nodule” may not manifest itself for several years - such a cavity is accidentally discovered during an X-ray or CT scan of the head.
However, when the size of the formation reaches 0.8 cm, the cyst already occupies an impressive part of the sinus volume, but does not extend beyond its limits. This is expressed in symptoms such as:
- heaviness and/or pain in the area of the affected sinus (sinus), aggravated by bending over, immersion in water (with changes in pressure);
- difficulty breathing, a feeling of nasal congestion - aggravated by physical activity or sleep - not everyone experiences this symptom;
- frequent exacerbations of inflammation of the frontal or maxillary sinuses, accompanied by purulent discharge;
- impaired perception of smell (hyposmia) or its complete absence (anosmia).
When it reaches a significant size (the cavity can increase to 300 ml or more in volume and push back the eye orbit), the symptoms of a cyst in the frontal sinus are as follows:
- displacement and protrusion of the eyeball, changes in the shape of the palpebral fissure, in rare cases, swelling of the eyelid - often it is ophthalmological symptoms that prompt a person to consult a doctor;
- impaired mobility of the eye muscles (if the tumor compresses the oculomotor nerve), discomfort when blinking, lacrimation;
- manifestation of double vision, decreased vision (with compression of the optic nerve), changes in color perception;
- swelling over the affected sinus of moderate density, not fused with the skin (the skin over the cyst is unchanged);
- Crepitation is characteristic - a phenomenon when the crunch of paper is heard during palpation of the neoplasm;
- when palpated, the cyst may be painful;
- pain in the lower forehead, radiating to the eye socket, upper jaw and teeth.
A mucocele can independently break into the nasal cavity (forming a fistula), however, this does not lead to a cure. In some cases, infection of the cavity occurs through the fistula tract.
Diagnostic measures
For an initial examination, you should contact an otolaryngologist . The doctor will need comprehensive information about the factors that could provoke the appearance of the tumor - if there have been injuries or severe inflammation in the past, this should be mentioned.
Rhinoscopy (examination of the passages using a mirror) is not effective in all cases - it may not reveal any changes. Among the more informative studies:
- Diaphanoscopy - transillumination of the frontal sinuses with an electric light bulb. If the anatomically frontal sinuses are symmetrical, and one is darkened, this allows one to suspect the presence of inflammation or a neoplasm.
- X-ray - reflects an increase in the size of the sinus (provided that the cyst has occupied more than 2/3 of the volume), a decrease in the transparency of the contents. The septum between the frontal sinuses can bend towards the healthy sinus. Based on the study, it can be assumed that there is an internal fistula in the posterior wall of the sinus.
- Probing of the nasal sinuses is carried out to determine the patency of the canals connecting the frontal sinuses and the nasal cavity. The procedure is performed under local anesthesia with a Lansberg cannula probe.
- Ultrasound of the frontal sinuses is an accessible and informative study that makes it possible to detect the presence of a neoplasm and changes in cartilage tissue.
- CT – high-resolution layer-by-layer radiography, allows you to diagnose the degree of the inflammatory process, the presence of a cyst (the level of density of its contents), accompanying bone changes, as well as the presence of structural anomalies or traces of injury.
- MRI - prescribed in case of discrepancy between symptoms and the results of previous studies, makes it possible to exclude general inflammation of the brain or orbit.
A diagnostic puncture is performed through the nasal passages, the contents either flow out freely or are pumped out and then sent for histological examination.
If there are pronounced ophthalmological symptoms, the following is carried out:
- testing visual acuity and color discrimination;
- ophthalmoscopy – examination of the fundus and optical media of the organ of vision;
- biomicroscopy of the conjunctiva, lens and membranes of the eye using a slit lamp.
The purpose of diagnosis is to identify and differentiate cysts from inflammation of the frontal sinuses, malignant neoplasms, and syphilis.
Treatment methods
Cysts of the frontal sinus with bone changes, regardless of the contents (sterile or purulent) and complications, require surgical removal. In elderly and weakened patients, it is possible to carry out a simplified version of the intervention - therapeutic puncture.
Drug therapy in the postoperative period is necessary to prevent complications . As an independent measure, conservative treatment of a cyst can be carried out only at an early stage of its development.
Drug treatment
The use of drugs, both oral and local, is reasonable only at the initial stage of cyst formation. Medicines are able to:
- eliminate the factor that creates obstacles to the outflow of secretions;
- reduce swelling and inflammation;
- improve sinus ventilation, reduce the concentration of toxins and bacterial flora;
- slow down the degenerative processes of the mucous membranes (after injury or inflammation);
- reduce pain syndrome.
Conservative therapy involves the use of the following groups of drugs:
- Topical antibacterial drugs (drops, aerosols) are effective at the initial stage of development of frontal sinusitis (Dioxidin, Bioparox, Mupirocin, Polydexa).
- Antibacterial agents for oral administration - for severe inflammation (Macropen, Zitrolide, Amoxiclav, Cefepime).
- Drugs that have a mucolytic effect - thinning the viscous secretion and promoting its outflow naturally (Rinufluimucil, Sinuforte, Sinupret, Mukodin, Nazivin).
- Vasoconstrictor drops and sprays - help relieve swelling (including allergic nature), improving sinus ventilation. If the swelling is insignificant, Galazolin, Otrivin, Sanorin drops are prescribed. For severe, prolonged hyperemia, use heavier drops of Midrimax, Nazivin, Nazol, Irifrin.
- Sprays with a moisturizing effect - help to slightly reduce swelling and wash out mucus, preventing drying of the nasal mucosa, removing allergens and pathogenic flora (Dolphin, Aquamaris, Otrivin-more, Aqualor).
In addition to medications, physiotherapy (Infrared therapy, UHF) is prescribed.
In rare cases, timely conservative therapy can avoid surgery.
Surgery
Radical techniques are the only way out in the presence of cysts that extend beyond the sinus, as well as complicated cavities.
Surgical removal is carried out using two main techniques . Traditional open surgery (frontotomy) involves making a skin incision along the length of the eyebrow. This is followed by sanitization of the cavity from mucus and pus with the installation of internal drainage.
The drainage is removed only after 14–21 days, when scars have formed. This is important for creating a stable connection between the frontal sinus and the nasal cavity. Disadvantages of the intervention include:
- inevitable injury to the skin and soft tissues;
- In general, endotracheal anesthesia is necessary:
- long-term rehabilitation;
- risk of infection and bleeding;
- the presence of a postoperative scar on the skin.
An alternative is endoscopic removal of the cyst through the nasal passage (without incisions). The procedure can be performed on an outpatient basis, the main advantages include:
- healthy tissues are practically not damaged;
- minimal blood loss;
- Application (1st stage) and local (2nd stage) anesthesia is sufficient;
- absence of postoperative defect in the form of a scar.
The disadvantage of endoscopic operations is the high probability of relapse (compared to frontotomy).
Regardless of the type of intervention, the patient requires rehabilitation after surgery (usually for 21 days), he is prescribed:
- taking antibacterial, anti-inflammatory and vasoconstrictor drugs;
- attending scheduled consultations with control diagnostics;
- refusal of physical activity, visiting a bathhouse or sauna.
In weakened or elderly patients, therapeutic puncture with aspiration can be performed - suctioning out the contents of the cyst and washing the cavity. However, the technique is used only if there are contraindications to radical operations, since it threatens relapses and the formation of a non-healing fistula.
Possible complications
In the absence of diagnosis and treatment of the cyst, the growth of the cavity leads to the formation of a fistula , through which the contents penetrate into adjacent tissues and structures. If the contents were infected (purulent), this provokes serious consequences:
- endophthalmitis - an acute inflammatory process in the internal structures of the eye with suppuration of the vitreous body;
- panophthalmitis - purulent inflammation of all membranes and elements of the organ of vision, threatening the loss of the eye;
- blockage and inflammation of the veins of the orbit;
- purulent inflammation of the fatty tissue around the eye - phlegmon (orbital cellulitis);
- suppuration of the bone tissues of the nose and orbit;
- inflammation of the meninges (meningitis) and brain (encephalitis) - in rare cases.
Complicated cysts significantly complicate surgical intervention (especially with regard to ophthalmological consequences); the prognosis for recovery and subsequent quality of life in such patients is less favorable.
A cyst in the frontal sinus cannot become malignant, however, its proximity to the nerves, organs of vision and brain structures requires the most careful attention to the characteristic symptoms.
Prevention should not be neglected - normalization of nasal breathing, strengthening of the immune system, adequate treatment of inflammation.
A complicated cyst not only complicates surgical treatment, but also threatens vision-threatening complications.
Source: https://KistNet.ru/lor/kista-v-lobnoj-pazuhe