Methods of treating the disease in the hospital
Sinusitis in different cases has varying degrees of severity. If the disease is not acute, the otolaryngologist will usually prescribe treatment at home, but when it comes to its purulent form, then in this case it is necessary to be treated in a hospital.
The disease goes away faster with complex therapy. At an appointment in a clinic, the doctor examines the patient and inquires about the symptoms present in the disease. Then he sends you for examination, and when the results appear, he makes a final diagnosis. After this, he prescribes a therapeutic course.
Previously, for sinusitis, the main method of treatment was puncture (puncture of the nasal sinus). Today, there are more innovative therapies available in the hospital. Mostly doctors prescribe:
- Rinsing the maxillary sinuses using the “cuckoo” technique.
- The use of antibacterial drugs if the disease is of bacterial origin.
- Relieving symptoms of pathology with the help of painkillers and antipyretics (Paracetamol, Ibuprofen) and vasoconstrictor medications (Tizin, Sanorin).
- Moistening the nasal passages with saline.
- Use of physiotherapy.
When the disease is more severe, the otolaryngologist may prescribe a puncture or surgery. Systematic medical monitoring and the ability to timely monitor the results of therapy will help to quickly cure sinusitis in a hospital setting. Treating sinusitis in a hospital will reduce the risk of serious complications.
Flushing or "Cuckoo"
During treatment of sinusitis in the hospital, lavage of the maxillary sinuses is often used. Popularly it has a simple name - “Cuckoo”. Scientifically, this method sounds like “Proetz fluid movement.”
“Cuckoo” is prescribed by doctors for the following ailments:
- severe rhinitis;
- damage to the sinuses of bacterial origin (sinusitis, sinusitis or frontal sinusitis);
- in the presence of pronounced adenoids;
As a result of the procedure, allergens and viral infections are eliminated from the nasal cavities. At the same time, inflammatory processes, itching, sneezing pass, and the sense of smell is acquired. This method is so effective that in most cases puncture can be avoided. This manipulation is safe and has a minimum of restrictions. It is carried out using an ENT combine.
See also
Which helps better with sinusitis and persistent runny nose in children and adults, “Isofra” or “Polydex” and the differences between antibiotics
Read
To rinse the nose, the doctor takes the following aids:
- drops with a vasoconstrictor effect;
- antiseptic;
- twenty cc syringe.
Before performing the procedure, 20 minutes before, you should drip vasoconstrictor drops into your nose. Then, through one nostril, the doctor slowly pours a warm antiseptic solution. On the other side of the nose, the device sucks out a viscous secretion with pathogenic microflora, which is contained in each maxillary sinus. During the session, the patient must say the phrase “ku-ku” so that the liquid does not enter the respiratory tract. For most patients, the optimal number of procedures is considered to be from 4 to 10.
After manipulation, the nasal mucous membranes are moistened with saline solutions.
“Cuckoo” is not recommended for people with epilepsy, as well as those suffering from frequent nosebleeds. The procedure is prohibited for children under 5 years of age.
Antibiotic therapy
When the previous method does not work, the doctor decides to use antibiotic therapy. Medicines can be prescribed to the patient in the form of injections, tablets or spray. Injections are used most often as this form of medication is the most effective.
Sometimes, if you are intolerant to antibiotics, your doctor may prescribe sulfa drugs. The doctor must determine the dosage and duration of use on an individual basis. He takes into account the neglect of the disease and the physiological characteristics of each patient. These medications have many contraindications.
Groups of antibiotics that are suitable for prescription by doctors without preliminary test results:
- Penicillins.
- Cephalosporins.
- Macrolides.
The last two groups are prescribed if the patient has an allergic reaction to the first. And to eliminate swelling in adults, you need to use a corticosteroid in the form of a spray.
Physiotherapy
They treat sinusitis without a puncture in combination with physiotherapeutic procedures. They are done only after clearing the sinuses of the contents.
Basic manipulations:
- Vibroacoustic treatment.
- Ultraviolet irradiation.
- Irrigation of the nasal cavity with medicine using ultrasound.
- Laser therapy.
- UHF of the maxillary sinuses.
Since each of the listed procedures requires the use of complex equipment, they are carried out only in a hospital setting.
Piercing method
This treatment method is used when purulent mucus is detected in the maxillary sinuses. The resulting substance should be removed quickly, since it is in close proximity to the brain, which is very dangerous. Using a puncture, you can get a fluid diagnosis result and disinfect the nasal sinuses.
See also
How and with what to treat sinusitis while breastfeeding?
Read
Indications for when a puncture is performed:
- prolonged headaches;
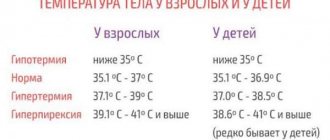
- the presence of an elevated temperature that is difficult to bring down;
- bilateral sinusitis.
The puncture method is still easier to tolerate by the patient than a complex surgical operation. The procedure is performed under local anesthesia and puncture. And the important thing is that you won’t have to stay in the hospital for a long time after it. The procedure is performed using a Kulikovsky otolaryngological needle. The doctor rinses the nasal passages with an antiseptic solution. Within 15 minutes, while the manipulation lasts, accumulations leave the maxillary sinuses.
Patients often ask how long to stay in the hospital after a puncture - this procedure is not very complicated, so a long stay in a hospital bed is not required.
Treatment of sinusitis at home and in the hospital
This unpleasant disease can trap each of us, regardless of lifestyle. Acute sinusitis, the treatment of which was untimely or delayed, can be fraught with complications. To avoid them, you must strictly follow your doctor’s advice. But, in addition to visiting the clinic, parallel treatment of sinusitis at home is no less important. This means both compliance with the regime and the use of some folk remedies as supportive ones.
Treatment of sinusitis at home and in the hospital
A painful sinus piercing is something that many patients want to avoid. Let's try to understand how necessary this measure is. Inflammation of the paranasal sinuses can occur due to a prolonged runny nose, a lingering cold, or an advanced viral infection. One of the little-known, but quite common reasons is problems with the upper teeth - purulent pulpitis can lead to the need for treatment of sinusitis. At home, this disease is easy to diagnose based on a number of symptoms. In addition to the nasal congestion that accompanies any runny nose, headaches appear (most often they are localized in the area of the bridge of the nose, forehead and temples), and high fever. A characteristic sign of sinusitis can be called loss of smell - even strong odors cease to be perceptible.
The headache gets worse in the evening. First, the patient feels it in the forehead, then it spreads even to the crown and back of the head. The general condition of the body also deteriorates - fatigue increases, concentration decreases, and it is difficult for a person to perform even light physical work. Due to the fact that the nose is constantly stuffy, a full supply of oxygen to the brain becomes impossible. If you do not start treating sinusitis at this moment, at home or in the hospital, it will go into a purulent stage. And this is much more dangerous and can have serious consequences, including frontal sinusitis and meningitis. Pharmacotherapy brings relief in cases of acute sinusitis. A course of antibiotics can quickly improve your general condition. Often used to cleanse the paranasal sinuses using puncture (puncture). If sinusitis has not become chronic, then this procedure is followed by rapid relief. It is important to understand at what stage the disease is.
Sinusitis. Traditional methods of treatment
After examination and consultation with a doctor, it is possible to use some proven methods at home. The main thing is that they do not contradict the general course prescribed by the specialist. Treating sinusitis at home using folk remedies can help improve the general condition of the patient. An effective remedy is heating - with a boiled egg wrapped in a clean cloth, or with a blue lamp (Minin reflector). However, if sinusitis has reached the purulent stage, this method can cause significant harm. Drops from aloe or Kalanchoe juice are considered harmless and effective. Honey inhalations are carried out as follows: put honey and anesthesin into hot water and breathe in the steam rising above this mixture until it cools. Such procedures are very effective and have no side effects.
fb.ru>
Surgical intervention
The most severe way to treat inflammation of the maxillary sinuses is surgery. It is carried out when the following factors are present during therapy:
- Previous treatments were not effective.
- The patient has odontogenic sinusitis.
- There is a polypous form of inflammation of maxillary sinusitis.
When the need arises, doctors open the source of inflammation and remove the affected sinus tissue. The surgical intervention is performed using general anesthesia and lasts 40-90 minutes.
Access to the maxillary sinuses is through the oral cavity or from the outside. In the second case, the scar after the operation will be almost invisible.
Today, surgical intervention using a special endoscope is widespread. This innovative method allows the operation to be performed in a more gentle manner. In this case, general anesthesia is used, and an endoscope is used to suck out the accumulation of pus, remove damaged tissue, and restore drainage.
Sinusitis
Sinusitis (sinusitis) is an acute or chronic inflammation of the sinuses, accompanied by headache, difficulty in nasal breathing, nasal discharge, decreased sense of smell, malaise, weakness, and increased body temperature. Diagnostics
examination of ENT organs, rhinoscopy; X-ray of the paranasal sinuses; computed tomography of the paranasal sinuses (if indicated); nuclear magnetic resonance (according to indications); bacterial culture for microflora and sensitivity to antibiotics; mucus microscopy; allergological and immunological examination; identification of concomitant diseases of the ENT organs.
Treatment
Conservative treatment of sinusitis (sinusitis): puncture of the paranasal sinuses with the administration of anti-inflammatory drugs;
nasal rinsing using the Politzer method (“Cuckoo”); anemia of the nasal mucosa; intranasal blockades; nasal shower; mucus suction; rinsing the maxillary sinuses through drainage with the administration of medications; ozone therapy; laser therapy (8-10 sessions per 1 course); Surgical treatment of sinusitis (sinusitis):
septoplasty (correction of the nasal septum); radioturbation of the nasal concha; submucosal vasotomy of the inferior turbinates; conchotomy; nasal polypotomy; minimally invasive endoscopic operations.
Advantages :
painless treatment; treatment without punctures and punctures.
Result
: normalization of nasal concha; restoration of smell; reduction in the number of exacerbations; improvement of general well-being.
Treatment of snoring
The causes of snoring (from the ENT organs) are: hypertrophy of the small uvula sagging soft palate adenoids vasomotor (allergic) rhinitis hypertrophy of the palatine tonsils curvature of the nasal septum
The classic causes of snoring are hypertrophy (enlargement) of the small uvula and sagging of the palate. Our radio wave technique allows us to eliminate these causes. The operation to treat snoring is outpatient, painless, bloodless and one-time.
CHRONIC TONSILLITIS
– a general infectious-allergic disease with a predominant localization of the process in the palatine tonsils. The disease occurs with periodic exacerbations, sore throat when swallowing, enlarged and painful submandibular lymph nodes, bad breath, and general intoxication of the body. Chronic tonsillitis complicates the course of other ENT diseases. With tonsillitis, complications are possible on local organs (peritonsillar abscess) and distant organs and systems (pyelonephritis, myocarditis, thyrotoxicosis, arthritis, prostatitis, skin diseases, peripheral nerve damage).
Diagnostics:
detection of pathological contents in the tonsils, bacterial culture of the oropharyngeal mucosa for flora and sensitivity to antibiotics, analysis of oropharyngeal mucus for fungal flora, microscopy of oropharyngeal discharge, study of immune and allergological status, blood and urine tests, electrocardiography (ECG), identification of concomitant diseases
Treatment:
conservative: washing the lacunae of the tonsils with antiseptic solutions, lubricating the oropharyngeal mucosa with wound-healing, emollient, anti-inflammatory drugs. Immunostimulating therapy (general and local), anti-inflammatory therapy (general and local), hyposensitizing agents, homeopathic treatment, pharyngeal blockades, vitamin therapy - In cases where conservative therapy does not bring the expected effect, the otorhinolaryngologist decides on surgical intervention.
Surgical:
Bilateral tonsillectomy - removal of the tonsils under local anesthesia.
Radio wave treatment - removal of palatine tonsils using the Surgitron device. The radio wave surgery method allows patients to avoid a difficult postoperative period; during the operation, Surgitron simultaneously cuts, stops the bleeding and disinfects the incision site. Advantages:
painless procedures, individual approach to each patient; the choice of therapy is made taking into account the results of bacterial cultures, studies of immune status and allergy anamnesis.
Efficiency:
complex conservative therapy - lasting results for many years. As a result of the treatment of tonsillitis, the number of exacerbations and acute respiratory diseases decreases, bad breath and throat discomfort are eliminated, the size of the palatine tonsils and submandibular lymph nodes decreases, and overall well-being improves. In the process of treating tonsillitis, complications on other organs and systems are prevented.
PHARYNGITIS
– acute or chronic inflammation of the pharyngeal mucosa. Causes of pharyngitis: the introduction of an infectious agent (viruses, bacteria, fungi) the influence of various unfavorable environmental factors (hypothermia, irritating effects of chemical and biological substances, exposure to allergens, prolonged vocal stress) concomitant diseases of the ENT organs (tonsillitis, rhinosinusitis, adenoids) presence other infectious diseases (tuberculosis, syphilis, herpes, mycosis) pathology of the gastrointestinal tract. introduction of an infectious agent (viruses, bacteria, fungi)
Diagnostics:
examination of the pharynx, bacterial culture from the mucous membrane of the oropharynx for flora and sensitivity to antibiotics, study of immune status, clinical and biochemical blood tests, microscopy of oropharyngeal discharge.
Treatment:
Conservative anti-inflammatory therapy (general and local) taking into account the microflora, washing the lacunae of the tonsils with antiseptic solutions, lubricating the back wall of the pharynx with wound-healing drugs, injections of biostimulants into the lateral ridges of the pharynx. immunostimulating and hypoallergenic therapy are aimed at increasing immunity and eliminating the allergic reaction. In order to speed up treatment, the patient is recommended to exclude the influence of harmful factors: smoking, drinking cold water and food, alcohol, hypothermia. Surgery. Radio wave removal of granules on the back wall of the pharynx is performed.
Advantage:
painless treatment method, comprehensive and individual approach to each patient. improvement in well-being occurs in a short time.
Efficiency:
sore throat, discomfort and the feeling of a foreign body in the throat are eliminated, complete recovery or a decrease in the number of exacerbations per year.
RINITIS (runny nose
) - inflammation of the nasal mucosa with impaired nasal function, accompanied by difficulty breathing, decreased sense of smell, bouts of sneezing, snoring, and periodic nasal discharge. Acute rhinitis most often has a viral nature. Chronic rhinitis is divided into allergic and non-allergic (infectious, vasomotor, hyperplastic, medicinal, atrophic, rhinitis due to hormonal imbalance).
Diagnostics:
examination by an otorhinolaryngologist;
microscopy of mucous discharge from the nose; bacterial culture of nasal mucus for flora and sensitivity to antibiotics; blood tests (biochemical, clinical); blood tests (allergological and immunological); X-ray of the paranasal sinuses (if indicated). Treatment
Conservative method: instillation of medicinal substances into the nasal cavity;
anemization of the nasal mucosa; nasal shower; rinsing the nose using the moving method; mucus suction; intranasal blockades; drug therapy - local and general (anti-inflammatory, decongestant, hypoallergenic, immunostimulating); treatment of concomitant diseases of the ENT organs. Surgical method: radioturbination of the nasal turbinates; submucosal vasotomy of the turbinates; conchotomy; polypotomy (removal of polyps); removal of nasopharyngeal formations using the radio wave method. Advantages:
Unique equipment Consultation with specialists in related fields Quick cure
OTIT is inflammation of one or more parts of the ear.
Causes include infection with a sharp object (hairpin, toothpick), entry and accumulation of moisture in the external auditory canal, contact with water (during swimming), upper respiratory tract infection (runny nose, sore throat, pharyngitis, tracheitis, laryngitis).
Acute catarrhal otitis media is an inflammatory infectious process in the tissues of the tympanic cavity, auditory tube and mastoid process. The incidence of acute otitis media is 25-30% of all ear diseases; the disease is more common in children and the elderly.
Causes:
introduction of infection into the middle ear from the nasal cavity through the auditory tube.
improper blowing of the nose (through both nostrils, and not each in turn), sneezing, coughing, which increase the pressure in the nasopharynx, as a result of which the infected mucus forcibly overcomes the barrier, which is the auditory tube. anatomical predisposition - infants have an anatomically short and wide auditory tube, stay in a horizontal position, frequent regurgitation, the presence of adenoids. through the blood - hematogenously, for infectious diseases (measles, scarlet fever, tuberculosis, etc.). Symptoms:
ear pain (usually severe and gradually increasing), a feeling of fullness and congestion in the ear, decreased hearing, noise in the ear, increased body temperature.
Acute purulent otitis media is the result of an unfavorable course of catarrhal otitis media. The reasons for this are the same.
Symptoms:
increasing pain in the ear, fever for several days, symptoms of intoxication (pallor, weakness, fatigue), purulent discharge from the ear). The appearance of pus indicates its breakthrough through the eardrum.
Chronic otitis media
- most often develops from an acute one, but sometimes it can take a chronic course from the very beginning.
In these cases, dysfunction of the auditory tube does not occur immediately, but gradually (especially in chronic diseases of the upper respiratory tract). Symptoms:
congestion in one or both ears, decreased hearing, a feeling of heaviness in the head, noise in the ear, autophony (resonance of one’s own voice in the affected ear), the sensation of iridescent liquid in the depths of the ear when tilting and turning the head.
According to the clinical course and severity of the disease, chronic suppurative otitis media is divided into two forms: mesotympanitis and epitympanitis.
Mesotympanitis occurs in 55% of cases. With this form of otitis, the process mainly involves the mucous membrane of the middle and lower parts of the tympanic cavity, as well as the area of the auditory tube. With mesotympanitis, a intact, loose part of the eardrum and the presence of perforation are determined. Patients complain of periodic or constant suppuration from the ear and decreased hearing, in rare cases - a feeling of noise in the ear and dizziness. Ear pain occurs only when the process worsens; sometimes it appears with secondary ear diseases - diffuse external or limited external otitis.
Symptoms:
The discharge from the ear is purulent and mucous in nature. hearing is reduced due to damage to the sound-conducting apparatus. causes of exacerbation of the process may be a cold, water getting into the ear, disease of the nose, nasopharynx.
Under favorable conditions and appropriate treatment, after complete cessation of suppuration, small perforations may heal. Despite the favorable course, with chronic mesotympanitis it is possible to develop severe intracranial complications.
With epitympanitis, the inflammatory process is localized mainly in the supratympanic space - the attic; the perforation usually occurs in the loose part of the eardrum. Epitympanitis is characterized by a more severe course compared to mesotympanitis.
Symptoms:
periodic pain in the temporo-parietal region, sensations of pressure in the ear, mucopurulent discharge with an unpleasant odor, and sometimes dizziness occurs. auditory function with epitympanitis is sharply reduced. headache, paresis of the facial nerve, vestibular disorders The occurrence of headaches, paresis of the facial nerve, and vestibular disorders in a patient with epitympanitis is an indication for immediate hospitalization of the patient for examination and surgical intervention on the ear.
Adhesive otitis media
- the disease is a consequence of prolonged fluid retention in the middle ear cavity due to inflammation and disruption of the patency of the auditory tubes connecting the cavities of the middle ear and nose. As a result of the process, dense connective tissue, adhesions, and adhesions are formed, limiting the mobility of the auditory ossicles and leading to a decrease in air conduction of sounds. Symptoms: persistent and progressive hearing loss, tinnitus.
Otomycosis
- the disease is caused by the development of various types of mold and yeast fungi on the walls of the external auditory canal. The occurrence is facilitated by skin irritation due to prolonged moisture, previous purulent otitis media, and irrational use of antibiotics and hormones.
Symptoms:
inflammation of the skin, itching, pain, moderate liquid discharge of yellow, dirty black, gray-green color depending on the type of fungus.
Furuncle
external auditory canal - found only in the cartilaginous part of the external auditory canal, because only here there are sebaceous glands and hair. The mechanism of the disease is based on the penetration of infection into the glands and hair follicles when they pick the ears with a fingernail or various objects, especially during suppuration. It also occurs as a manifestation of general furunculosis in diabetes mellitus, hypovitaminosis, etc.
Symptoms:
severe pain in the ear, especially when pressing on the place where the auricle is attached. The lymph nodes behind the ear become enlarged and painful.
Bleeding from the ear
- the most serious bleeding from the ear is observed with fractures of the bone part of the ear canal and a simultaneous rupture of the eardrum. Other causes include acute and chronic suppurative otitis media, trauma and tumors of the middle ear and external auditory canal. If bleeding occurs, you should immediately consult a doctor.
Diagnostics:
examination by an otolaryngologist, otoscopy (examination of the eardrum), bacterial culture of ear discharge for flora and sensitivity to antibiotics, microscopy of ear discharge, hearing examination with tuning forks, otoneurological examination, examination of immunological status
Treatment:
anti-inflammatory therapy (general and local) immunostimulating therapy paracentesis of the eardrum, including using the radio wave method, shunting of the tympanic cavity, removal of benign tumors of the ear using the radio wave method, opening of the ear boil, removal of foreign bodies in the ear, catheterization of the auditory tube, washing the attic with medicinal substances, pneumomassage of the eardrum, Politzer blowing, ear toilet treatment concomitant ENT diseases
Advantages
Consultation with specialists in related fields Quick cure Effective techniques Individual approach
How long does hospital treatment take?
How many days the treatment of sinusitis in the hospital will last depends on the stage of development of the disease. At the initial stage of the acute form of the disease, the therapeutic course should last for 1-2 weeks, if the patient follows all the doctor’s recommendations. Most often, timely treatment lasts no more than 7 days.
After surgery using an endoscope, the patient will spend several days in the hospital and then will be treated at home.
If your attending physician insists on medical examination for sinusitis, then there is no need to refuse. Treatment in a hospital setting has advantages. There they can quickly prevent the development of complications. The duration of the therapeutic course rarely exceeds 14 days, and ends with complete recovery.
How long is sinusitis treated: how long do they stay in the hospital with sinusitis?
Like any disease, sinusitis has its own treatment periods, which vary depending on the type of disease.
However, it will be useful to know how many days sinusitis is treated in order to understand how much time will have to be spent on procedures, or how much time can be spent on sick leave.
Let us say right away that just as the treatment regimen is chosen individually, the treatment time may vary for each patient.
It is very important in this regard to consider sinusitis as an acute or chronic course of the disease.
In addition, the duration of treatment is directly influenced by the degree of neglect of the disease, the general condition of the patient’s body, the state of his immunity and concomitant diseases.
How does sinusitis go?
The standard treatment period for sinusitis ranges from one week to a month.
The disease itself is represented by an inflammatory process in the nasal sinuses. Inflammation affects either one or both maxillary sinuses or paranasal sinuses. For the development of the disease, a characteristic symptom is the appearance of mucus, but in some cases this does not happen. So the diagnosis must be carried out by a doctor.
If the disease develops without accumulation of pus, and inflammation was detected at the initial stage, then sinusitis can be cured in just a couple of days. And, nevertheless, even with such a mild form, it is preferable to consult a doctor.
The fact is that you may need not just medications, but also antibiotics, and taking antibacterial drugs on your own without a prescription or prescribed course is extremely dangerous.
If a hospital stay is required, the patient will be treated here:
- Physiotherapeutic treatment.
- Puncture as a minimally invasive treatment.
- Laser treatment.
- Special rinsing.
And the time that the patient will be treated for sinusitis depends on each chosen direction.
Time of diagnosis
As a rule, it will take 2 to 3 days to make an accurate diagnosis. Of course, even with a visual examination, the doctor can immediately determine the problem in general terms.
However, for an accurate diagnosis, to understand the spread of the inflammatory process and its nature, some laboratory tests will be required.
Among the symptoms to look out for are:
- Severe nasal congestion that does not go away with standard remedies.
- Difficult nasal breathing, or its complete absence.
- Pain in the bridge of the nose, forehead, headache that is difficult to relieve.
- Cloudy mucus, brown or pink snot.
- Increased body temperature.
After laboratory tests, a treatment regimen will be developed and antibiotics will be selected.
Treatment time in different situations
Let's start with a course of antibiotics.
In this case, the treatment time can last for at least 5 days. In principle, the first positive changes in the patient’s well-being can be noted within a day after starting antibiotics, but you should not stop taking them.
To treat a mild form, if it is, for example, catarrhal sinusitis, it will take a minimum of time, from 5 to 7 days. It will not be possible to speed up the process, but you can help with treatment by using nasal rinsing, for example, Cuckoo nasal rinsing.
In a more severe case, if it is purulent sinusitis in the acute phase, treatment will take a relatively long time. The problem with a purulent complication is that to completely cure it, sometimes several courses of different drugs are required, since the infection itself can be caused by several types of bacteria.
However, the duration of such treatment is also quite adequate; as a rule, it takes from 10 to 14 days to completely eliminate the problem of infectious inflammation.
How long to treat chronic disease?
If relapses of sinusitis occur more often than twice a year, we can talk about a chronic form of sinusitis.
The problem of the chronic form for the patient is that all pathogenic bacteria and microorganisms that cause inflammation in the sinuses are now practically resistant to antibacterial drugs.
The point is not that this type of disease always takes a long time to be treated, but that courses of antibiotics have to be constantly changed so as not to develop a kind of immunity in the disease to the active substances of the drugs.
This form of sinusitis is treated for 14 days, and then a recovery period begins, in which antibiotics are no longer used, but various physiotherapy procedures are used. This period may last several more weeks.
Allergic sinusitis
The allergic nature of sinusitis indicates that it was provoked by a variety of allergens.
Without identifying the allergen, treatment will not be effective. In addition, with frequent occurrence, this form of the disease begins to gradually reduce the patient’s immunity.
Unfortunately, this form of sinusitis requires long-term treatment and may take up to several months to completely heal.
The fact is that therapy here involves working in several directions, plus a general strengthening of the immune system and the body is necessary.
And during the period of exacerbation, it is necessary to use exclusively antiallergic drugs and antihistamines to alleviate the patient’s condition.
Advanced stage of sinusitis
In some cases, sinusitis can develop into complications if patients do not seek medical help for a long time.
Complications of sinusitis may be as follows:
- Pneumonia in two forms.
- Meningitis, pus can penetrate into the brain area.
- Inflammatory process of the heart muscles.
- Sepsis.
Such complications always lead to long and complex treatment. Plus, in extremely severe cases, the patient may end up in intensive care, and doctors will literally fight for his life.
In this condition, it may take several months to eliminate both the sinusitis itself and its complications. And the video in this article will demonstrate what sinusitis is, talk about its symptoms and terms of treatment.
stopgripp.ru>