Stenosing laryngotracheitis is an inflammation of the mucous membrane of the larynx and trachea with symptoms of laryngeal stenosis due to edema in the subglottic space. The clinical picture of stenosing laryngotracheitis is characterized by a triad of symptoms: barking cough, dysphonia, inspiratory stridor.
Stage 1 of stenosis (stage of compensated breathing): presence of signs of respiratory failure during physical activity, absence of signs of respiratory failure at rest. Stage 2 of stenosis (stage of incomplete compensation of breathing): the presence of signs of respiratory failure at rest. Stage 3 of stenosis (stage of respiratory decompensation): signs of respiratory failure are accompanied by signs of cardiovascular failure, and from the nervous system - agitation or inhibition. Stage 4 stenosis (terminal): development of hypoxic coma with further impairment of vital functions.
Emergency assistance procedure
Stage 1 stenosis:
a) provide access to fresh cool air; b) in the absence of fever, distracting procedures: mustard plasters on the calf muscles, warm foot or general baths (water temperature increased gradually from 37 to 40.C); c) in the absence of fever, warm inhalations with isotonic NaCl solution; d) warm, plentiful drink; e) administer 2% papaverine hydrochloride – 0.15 ml/year of life intramuscularly; f) for the allergic nature of the disease, antihistamines: 2.5% promethazine solution (pipolfen) - 0.1 ml/year of life intramuscularly.
Stage 2 stenosis:
a) provide access to fresh cool air; b) in the absence of fever, distracting procedures: mustard plasters on the calf muscles, warm foot or general baths (water temperature increased gradually from 37 to 40.C); c) in the absence of fever, warm inhalations with isotonic NaCl solution; d) administer 2% papaverine hydrochloride – 0.15 ml/year of life intramuscularly; e) for the allergic nature of the disease, antihistamines: 2.5% promethazine solution (pipolfen) - 0.1 ml/year of life intramuscularly; e) prednisolone 2-3 mg/kg intramuscularly; g) 0.1% solution of epinephrine (adrenaline hydrochloride) – 0.01 ml/kg subcutaneously (maximum dose 0.3 ml) with an interval of 5 minutes no more than 3 times. h) hospitalization.
3-4 stages of stenosis:
a) provide access to fresh cool air; b) administer 2% papaverine hydrochloride – 0.15 ml/year of life intramuscularly; c) for the allergic nature of the disease, antihistamines: 2.5% promethazine solution (pipolfen) - 0.1 ml/year of life intramuscularly; d) prednisolone at least 5 mg/kg intramuscularly; e) 0.1% solution of epinephrine (adrenaline hydrochloride) – 0.01 ml/kg subcutaneously (maximum dose 0.3 ml) with an interval of 5 minutes no more than 3 times; f) emergency hospitalization.
Acute respiratory viral infections (ARVI) are the most common diseases in children. In previous years, severe ARVI was more often accompanied by neurotoxicosis and pneumonia, and recently there has been a progressive increase in the incidence of acute stenotic laryngotracheitis (ASLT).
At the same time, symptoms of laryngotracheitis are observed in half of patients with ARVI, of which up to 75% of cases are with progressive symptoms of laryngeal stenosis. OSLT is more often observed in boys (up to 70%).
The incidence of OSLT depends on age: at the age of 6 to 12 months - in 15.5% of cases, in the second year of life - in 34%, in the third - in 21.2%, in the fourth - in 18%, over 5 years - in 11 .3%. Mortality in OSLT ranges from 0.5 to 13%, and in decompensated forms - from 3 to 33%.
Definition. Acute stenosing laryngotracheitis (ICD-10 J05.0) is an obstruction of the upper respiratory tract, having a viral or viral-bacterial etiology, accompanied by the development of acute respiratory failure and characterized by barking cough, dysphonia, inspiratory stridor and laryngeal stenosis of varying severity.
Clinical classifications of OSLT
1. Depending on the type of viral infection (influenza, parainfluenza, etc.).
2. According to the clinical variant: primary, recurrent.
3. According to the severity of the course: 1st stage - compensated, 2nd - subcompensated, 3rd - decompensated, 4th - terminal (asphyxia).
4. Depending on the clinical and morphological form of stenosis, the following are distinguished:
- edematous form of infectious-allergic origin, characterized by a rapid increase in stenosis in the acute period of ARVI;
- infiltrative form of viral-bacterial origin, in which stenosis develops slowly, but progresses to a severe degree;
- obstructive form, manifested by a descending bacterial process such as fibrinous inflammation of the trachea and bronchi.
An urgent situation arises as a result of the rapid transition of a compensated pathological process to the stage of decompensation.
First aid
Laryngeal stenosis is the main cause of seizures in young children. Regardless of the stage of development of the disease, when the first symptoms of false croup appear, you need to call a doctor at home. Only he will be able to adequately assess the patient’s condition and prescribe treatment on an outpatient or inpatient basis. How to help a child before the ambulance arrives?
Parents are not always able to promptly identify the symptoms of stenosing laryngotracheitis and consult a specialist. If an attack occurs, the patient must be given competent pre-hospital care. In an extreme situation, parents must remain absolutely calm so as not to frighten the child or aggravate his condition.
What to do first? In case of laryngospasm, you need to act according to a clear algorithm:
- provide bed rest;
- ventilate the room;
- use distraction therapy;
- give antipyretic drugs;
- put vasoconstrictor drops into the nose;
- provide plenty of fluids.
Important! With a spastic cough, children should not be given mucolytics, as they stimulate the production of mucus, which the child will not be able to cough up due to laryngeal stenosis.
In most cases, stenosing laryngotracheitis in children is quite easy to treat. However, the first attack of suffocating cough can greatly frighten not only the child, but also his parents. Therefore, before the ambulance arrives, you need to strictly follow the instructions and correctly perform all the necessary manipulations.
Clinical manifestations of laryngotracheitis
Clinical manifestations depend on the etiological variant, the severity of the stenosis and the age of the child.
To assess the severity of OSLT in international pediatric practice, the Westley scale is used.
For mild stenosis - less than 2 points; for moderate stenosis - from 3 to 7 points; with severe stenosis - more than 8 points.
Differential diagnosis is carried out with laryngeal diphtheria, congenital stridor, epiglottitis, spasmophilia syndrome with laryngospasm, foreign body of the upper respiratory tract, laryngeal injuries, Ludwig's tonsillitis, retropharyngeal and paratonsillar abscesses, mononucleosis, papillomatosis of the larynx and trachea.
Antipyretics
High temperature stimulates sweating and leads to dehydration of mucous membranes. In addition, low-grade fever provokes increased breathing, which leads to drying of the mucous membranes of the ENT organs and exacerbation of respiratory failure. If body temperature exceeds 38-38.5 degrees, it is recommended to use antipyretics.
In pediatric practice, Nurofen for children, Ibuprofen, Paracetamol, and Vibrukol are used to reduce fever. If the barking cough does not stop, it is advisable to use antipyretics in the form of rectal suppositories. The safest drugs include Panadol, Efferalgan and Cefekon.
If a child experiences febrile seizures, you should immediately call an ambulance. It should be remembered that any antipyretic drugs that contain acetylsalicylic acid should not be given to children under 12 years of age. Failure to comply with this rule may cause the development of Reye's syndrome, in which the patient experiences cerebral edema and liver failure.
Indications for hospitalization for laryngotracheitis
- all cases of stenosis of degree II or more;
- patients with grade I stenosis due to congenital stridor, epilepsy and other aggravating factors;
- children 1 year of age and extremely premature according to medical history;
- children from socially disadvantaged families;
- impossibility of providing constant dynamic medical monitoring of the condition of a child with OSLT.
Acute stenotic laryngotracheitis (false croup) is an inflammation of the mucous membrane of the larynx and trachea with symptoms of stenosis due to edema in the subglottic space and reflex spasm of the laryngeal muscles. It most often develops in children under 3 years of age.
How does croup syndrome manifest?
The first clinical manifestations of stenosing laryngotracheitis are identical to the symptoms of a cold. Children complain of nasal congestion, runny nose, fever, lethargy and occasional cough. If the problem is ignored and there is no treatment, after 2-3 days the above-mentioned symptoms are joined by specific signs indicating the development of false croup:
- hoarseness and nasal voice;
- dry barking cough;
- inspiratory dyspnea;
- whistling when exhaling and inhaling;
- nervous overexcitement.
As a rule, laryngospasms occur in children in the evening before bedtime. The child becomes whiny and restless, breathes heavily, often tosses and turns and coughs.
Due to the lack of oxygen in the body, the skin becomes very pale, and cyanosis (blue discoloration) of the lips occurs. Rapid shallow breathing is a good reason to call an ambulance to your home.
Clinic.
It occurs suddenly, often at night against the background of acute respiratory viral infections, catarrhal symptoms, and elevated body temperature.
I degree (compensated stenosis). Moderate condition. Consciousness is clear. The child is restless and cannot find a comfortable position in bed. Periodically, with anxiety, inspiratory shortness of breath and barking cough are noted. At rest, breathing is even. The voice is hoarse. Skin of normal color. Heart rate exceeds the age norm by 5-10%.
II degree (subcompensated stenosis). The general condition is serious. The child is excited, restless, and sleep is disturbed. Noisy breathing is interrupted by bouts of rough barking cough. Inspiratory dyspnea increases with retraction of the compliant areas of the chest, jugular fossa, and flaring of the wings of the nose. The voice is hoarse. The skin is pale with perioral cyanosis. Heart rate exceeds the norm by 10-15%.
III degree (decompensated stenosis). The child's condition is very serious. Excitement gives way to lethargy, confusion is possible. Inhalation is sharply difficult with retraction of the sternum and the participation of auxiliary muscles, exhalation is shortened. Skin with mucous membranes is pale, sometimes sallow in color, acrocyanosis, cold sweat. Symptoms of circulatory failure are expressed: marbling of the skin, tachycardia, muffled heart sounds, frequent weak arrhythmic pulse.
IV degree (asphyxia). The condition is extremely serious. There is no consciousness, the pupils are dilated, convulsions are possible. Breathing is shallow, silent (imaginary well-being). The skin is cyanotic. Bradycardia, muffled heart sounds, thready or undetectable pulse. Respiratory and cardiac arrest.
Help in the first minutes
In the first minutes after an attack occurs, it is undesirable to force the child to perform any procedures. Physical activity will only worsen the child’s well-being and make breathing difficult. How to act in such a situation? First of all, you need to lay the child down and place a blanket or several pillows under his back.
To prevent your child from panicking due to lack of oxygen, try to calm him down. Fear only intensifies the spasm of the muscles of the larynx, stimulates increased breathing and thereby prolongs the attack.
Explain to your child that at rest, shortness of breath will quickly go away and his breathing will return to normal.
A barking cough appears due to dryness and irritation of the mucous membrane. To reduce symptoms, provide access to fresh air. If signs of false croup increase, open windows, doors and humidify the air. If you don't have a special humidifier, spray saline or mineral water in the room. It is advisable that the air temperature in the room does not exceed 20 degrees.
Traditional medicine treatment
At the initial stage, stenosing laryngotracheitis can be treated using traditional medicine, but only after consultation with your doctor.
For this treatment, you can use the juice of aloe, carrots and honey; the patient should drink 1 teaspoon of this mixture before meals; warm milk with a pinch of soda and a teaspoon of honey is also recommended twice a day.
This disease should only be treated by a doctor who can not only establish the correct diagnosis, but also prescribe the correct treatment to the patient, which will not lead to complications.
Source
Alternative therapy
The main task of emergency care is to reduce swelling of the mucous membranes and restore normal patency of the respiratory tract. In many ways, the principles of first aid depend on the stage of laryngeal stenosis. It should be noted that for stenosis at stages 3 and 4 of development, treatment is carried out only in a hospital setting using oxygen therapy.
Emergency prehospital care, taking into account the stage of development of laryngeal stenosis:
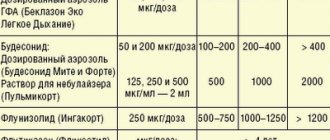
| Stage of laryngeal stenosis | Clinical manifestations | Drugs used |
| 1 (compensated stenosis) |
|
|
| 2 (subcompensated stenosis) |
|
|
| 3 (decompensated stenosis) |
|
|
| 4 (terminal stenosis) |
|
|
If there is no effect from the use of drugs, tracheal intubation may be required. While transporting the child to the intensive care unit, doctors perform infusion therapy, which involves intravenous administration of medicinal solutions that support the patient’s vital functions.
First aid and first aid
When an adult exhibits all the symptoms indicating laryngitis, it is necessary to immediately call a doctor. While waiting for an ambulance, you should ventilate the room, and if breathing is very difficult, perform first aid.
To do this, you should perform steam inhalation using anti-inflammatory herbs such as chamomile or eucalyptus. But they can be used only in the absence of allergies and fever. If there are no herbs, then fresh boiled potatoes in their jackets can replace them. While waiting for the doctor, the patient can drink warm water or tea with the same herbs.
Upon arrival of the doctor, first aid is provided immediately; for this, Papaverine hydrochloride is injected intramuscularly. And if you are prone to allergies, an additional injection of Promethazine is given.
If stage 3 or 4 of the disease is diagnosed, Epinephrine solution is administered at intervals of five minutes. The injection is given subcutaneously no more than three times.
If the doctor diagnoses acute stenosing laryngotracheitis in the patient, immediate hospitalization is carried out and further treatment is carried out in the hospital.
Vasoconstrictor drops
Stenosing laryngotracheitis very often develops against the background of viral, bacterial or allergic rhinitis. To facilitate nasal breathing in a child, it is recommended to use vasoconstrictor drugs. They will reduce the permeability of blood vessels and thereby eliminate swelling in the respiratory tract.
The following can be used as vasoconstrictors:
- "Tizin Xylo";
"Otrivin Baby";- "Nazivin";
- "Advance spray";
- "Adrianol."
Important! It is undesirable to instill vasoconstrictor drops into the nose with severe tachycardia and atrophic runny nose.
After eliminating the symptoms of false croup, you need to seek help from a specialist. It should be understood that without adequate treatment, the symptoms of the disease will only worsen, which can cause acute respiratory failure and hypoxic coma.
Drug treatment
In the hospital, treatment is carried out with medications that are prescribed by a doctor depending on the degree to which acute stenosing laryngotracheitis occurs.
Antiviral drugs are used only if OSLT is not caused by a complex infection. In this case, laryngeal stenosis is alleviated within 48 hours from the moment of taking the drugs. To achieve greater results, additional introferons may be prescribed. This type of drug is very common for the treatment of childhood diseases, since the immune system is not yet able to cope with the virus on its own. These drugs include:
- Ergoferon;
- Viferon;
- Cycloferon;
- Ingavirin.
If the disease was caused by a bacterial infection, then treatment is carried out with broad-spectrum antibiotics. The concentration and method of administration are selected individually for each individual, depending on the complexity of the disease and the age of the patient. Antibiotics administered:
- Flemoclav;
- Amoxiclav;
- Klacid;
- Suprax;
- Sumamed.
To relieve swelling of the larynx, the patient is prescribed glucocorticosteroids. GCS is no longer prescribed in pediatrics, since these drugs have an extensive list of side effects. Edema is relieved by inhalation, using the relatively new drug Berodual. This remedy is highly effective and quickly relieves complications of the disease.
Acute stenosing laryngotracheitis can be treated with antihistamines. They relieve swelling of the larynx in a short time and act on the component of inflammation that was caused by allergies. This type of medication is common for treating illness in children who are prone to allergies. In some cases, diuretics may be used.
If the disease is with laryngeal stenosis, then you cannot do without muscle relaxants, but they are used only if there is a pronounced possibility of complications.
These complications include:
- relaxation of respiratory muscles;
- suppression of the cough reflex;
- depression of the respiratory center.
These complications negatively affect the body, since the immune system is already greatly weakened. They can lead to severe stagnation of sputum, as a result of which it will begin to settle in low respiratory areas and cause bronchitis or pneumonia.
Your doctor may also prescribe expectorants to help clear mucus without irritating your larynx and vocal cords. Cough medications prescribed for stenosing disease:
- ACC;
- Lazolvan;
- Linux;
- Sinekod.
To reduce body temperature, use Paracetamol or Nurofen.
In the hospital, steam oxygen therapy will also be carried out, and in case of acute stenotic laryngotracheitis - nasotracheal intubation.