What is Staphylococcus aureus?
Staphylococcus aureus is a gram-positive spherical bacterium that causes a wide range of different diseases: from mild acne to severe staphylococcal sepsis. Almost 20% of the population are its carriers, parasitizing the mucous membrane of the upper respiratory tract or skin.
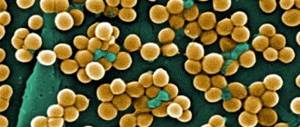
Staphylococcus aureus gets its name from the golden glow it produces when sown on a nutrient medium. Translated from the Greek slaphyle - “bunch” and coccus - “spherical”, staphylococcus under a microscope resembles a bunch of grapes.
The pathogenic microorganism is active in the body of both children and adults. But if the body’s immune system works stably, then normal microflora suppresses the activity of these bacteria. If the body's reactivity weakens, the microbe becomes more active and provokes the progression of pathologies.
Features of Staphylococcus aureus:
- the bacterium is resistant to various antiseptics, and also does not die for a long time when boiled, frozen, dried, etc.;
- do not form a dispute.
- Bacteria are very picky about environmental conditions. The optimal air temperature for their active development is 30-37 C, the acid-base balance should be neutral.
How is treatment carried out in children and pregnant women?
If we consider that one of the prerequisites for the active spread of infection is weak immunity, then young children and pregnant women are immediately at risk. But there are many restrictions on treatment, because it must not pose a health hazard or cause harm.
Of course, only the attending physician chooses the correct treatment regimen for staphylococcus in the throat. In addition, a pregnant woman may need more careful observation by a gynecologist, as well as his consultation.
The most basic limitation is that these categories of patients cannot take antibiotics. In such a situation, bacteriophages are used for treatment, as well as folk remedies: rinses, tinctures and proper nutrition.
Staphylococcus itself is not dangerous if you start treating it at the very first symptoms. Modern medicine has a wide range of solutions and drugs to get rid of infection. But if left untreated for a long time, severe complications can occur, even leading to death.
Staphylococci are gram-positive bacteria that humans encounter in the environment. Some of their species live in the body when favorable conditions are created or the immune system is disrupted.
The greatest threat to health is Staphylococcus aureus, which can live on the skin, mucous membranes of the nasopharynx, mouth and intestines. Staphylococci in the mouth and nose can cause certain symptoms and cause the development of dangerous pathologies.
Causes
The human immune system prevents staphylococcus from displaying its pathogenic properties. In a healthy body, it is able to withstand the onslaught of all pathogenicity factors of a given bacterium (enzymes, hemolysins, toxins, etc.). If local and general immune defense weakens, a staphylococcal infection develops.
Infection with Staphylococcus aureus occurs when immunity decreases, which is facilitated by a number of factors:
- taking antibiotics and hormonal drugs;
- stress;
- poor nutrition;
- hypo- and vitamin deficiencies;
- infections;
- intestinal dysbiosis;
- failure to comply with personal hygiene rules;
- prematurity;
- immaturity of the child at birth;
- artificial feeding;
- late breastfeeding.
By the way, strains of resistant, the most dangerous and terrible staphylococcus, insensitive to most known antibiotics, are called MRSA (from the English Methicillin-resistant Staphylococcus aureus - methicillin-resistant Staphylococcus aureus). Only people with a low immune response are likely to “catch” such an instance:
- patients with HIV (AIDS), cancer, severe asthma, diabetes;
- old people;
- patients after organ transplantation;
- patients taking corticosteroids for a long time, and others.
How is Staphylococcus aureus transmitted?
Transmission routes:
- Staphylococcus aureus is most often spread through contaminated hands.
- Healthy skin and mucous membranes are an effective barrier against infection. However, if these barriers are broken (skin damage due to trauma or mucosal damage due to viral infection), infection is allowed to enter the underlying tissues and bloodstream, causing disease.
- People who are immunocompromised or have invasive medical devices are particularly vulnerable.
The range of diseases caused by bacteria is striking in its diversity:
- Skin infections - carbuncles, boils, cellulitis, folliculitis, bullous impetigo.
- Respiratory tract infections - pneumonia, sore throat.
- Infections of the central nervous system - meningitis, brain abscess, thrombophlebitis of the superficial veins of the brain.
- Urinary tract infections – cystitis, urethritis.
- Infections of bones, joints, muscles - osteomyelitis, purulent arthritis, purulent myositis.
One of the negative features of Staphylococcus aureus is its resistance to treatment with many antibiotics, including penicillin. For this reason, it causes serious outbreaks of nosocomial infections.
Symptoms of Staphylococcus aureus
Specific clinical manifestations of staphylococcal infection depend on the site of introduction of the microorganism and the degree of decreased immunity in the patient. For example, in some people infection ends with a simple boil, and in weakened patients - with an abscess and phlegmon, etc.
General symptoms characteristic of Staphylococcus aureus in adults:
- fast fatiguability;
- general weakness;
- lack of appetite;
- aches in bones and joints;
- nausea and vomiting;
- increase in body temperature.
These are common signs of infection by harmful bacteria. Depending on the strength of the immune system and the resistance of the body’s systems, this list may be supplemented by other symptoms that more specifically indicate the type of disease.
Skin damage
Skin infections are characterized by rashes on the skin, the appearance of blisters with purulent contents, crusts, redness, and induration.
Infections of ENT organs and eyes
Getting on the mucous epithelium of the throat or nose, staphylococcal infection provokes the occurrence of sore throat, otitis media, sinusitis and other inflammatory pathologies of the ENT organs or upper respiratory tract.
When Staphylococcus aureus infects the lungs, staphylococcal pneumonia develops, characterized by the appearance of shortness of breath and chest pain, severe intoxication of the body and the formation of many purulent formations in the lung tissues, gradually transforming into abscesses. When abscesses break into the pleural cavity, suppuration of the pleura (empyema) develops.
When the mucous membrane of the eyes is damaged, conjunctivitis develops (photophobia, lacrimation, swelling of the eyelids, purulent discharge from the eyes).
CNS damage
If Staphylococcus aureus enters the brain, there is a high probability of developing meningitis or a brain abscess. In children, these pathologies are extremely severe and cases of death are not uncommon. Characteristic symptoms:
- intoxication syndrome;
- hyperthermia;
- severe vomiting;
- meningeal symptoms are positive;
- elements of a rash appear on the skin.
Staphylococcus aureus affects the genitourinary system
Urinary tract infection caused by Staphylococcus aureus is characterized by:
- urination disorder (frequency, pain),
- slight fever (sometimes there may be no fever),
- the presence of pus, blood admixtures and the detection of Staphylococcus aureus during general and bacteriological examination of urine.
Without treatment, staphylococcus can infect surrounding tissues (prostate gland, perinephric tissue) and cause pyelonephritis or form kidney abscesses.
Damage to the musculoskeletal system
This pathogen is the leading cause of purulent lesions of the musculoskeletal system (osteomyelitis and arthritis). Such pathological conditions develop more often in adolescents. In adults, staphylococcal arthritis often develops against the background of existing rheumatism or after joint replacement.
Food poisoning
It develops when eating contaminated or spoiled food and occurs with symptoms of acute enterocolitis. Characterized by fever, nausea, vomiting up to 10 or more times a day, loose stools mixed with greens.
Staphylococcus aureus is a dangerous type of bacteria that causes many infections when the patient’s immune system is weakened. If you notice the first general symptoms (lethargy, nausea, lack of appetite), you should immediately consult a doctor.
Symptoms of the appearance of staphylococcus
To quickly and easily get rid of the infection, you need to consult a doctor in time. And to do this, you should know what Staphylococcus aureus looks like in the throat.
In the first stages, the disease is similar to a common cold. But bacteria actively multiplying in the oral cavity and nasopharynx synthesize toxic substances and specific enzymes that kill cells and enhance the inflammatory response. So rhinitis gradually flows first into pharyngitis, tracheitis, bronchitis, and then into pneumonia.
A person can understand that a bacterial infection is developing in his body by the following symptoms:
- inflamed lymph nodes;
- high body temperature;
- dry mouth;
- muscle spasms;
- runny nose;
- unpleasant sensations in the throat;
- slight urge to vomit;
- painful incessant cough;
- lack of appetite;
- dizziness;
- inflamed tonsils;
- swelling of the oral mucosa;
- ulcers on the tongue.
- Staphylococcus aureus in the throat - symptoms, treatment;
- White lumps in the throat with an unpleasant odor - how to treat it;
- Cheap analogues of Amoxiclav - list with prices, which ones are better.
Diagnostics
If signs of inflammation appear in any organ, you should contact the appropriate specialist. If it is difficult to determine on your own what is affected in the body, consult a therapist or pediatrician. After diagnosis, the patient can be referred to a specialized specialist:
- surgeon (for abscesses of internal organs),
- dermatologist (for skin lesions),
- cardiologist, pulmonologist, traumatologist, rheumatologist, ophthalmologist, neurologist, dentist.
The standard diagnostic plan includes the following methods:
- latex agglutination;
- standard coagulase test in vitro;
- clinical and biochemical blood test;
- sowing of biological material;
- swab from the eyelid for suspected conjunctivitis;
- Widal agglutination reaction.
Depending on the type and location of the staphylococcal infection, the following are used as biological material:
- discharge of mucous membranes (most often in the nasopharynx);
- sputum;
- wound contents (pus and inflammatory exudate);
- blood (for sepsis);
- urine;
- feces;
- bile;
- cerebrospinal fluid
On nutrient media, Staphylococcus aureus forms smooth, convex, cloudy colonies with a diameter of about 4–5 mm. Such colonies are colored in various shades of yellow, which gives rise to the name of the pathogen.
Diagnosis of the disease
Coagulase test for staphylococcus
The final diagnosis is made by a doctor only after undergoing the necessary examination. There are two methods for detecting the disease - microbiological and serological.
The first method consists of taking a swab from the throat for the presence of bacteria and testing for their accumulation. For such sowing, as a rule, a simple nutrient medium is used, which has excellent pigmentation abilities. The first results can be noted within about a day: with ordinary staphylococcus, a yellowish pigment will remain behind, and golden pigment will appear in the form of colonies with a convex and cloudy shape, which has a white, yellow or orange color. Also today, a coagulase test is used, which makes it possible to determine the presence of bacteria much faster. It is carried out for only four hours, but if the result is negative, it is extended for another day.
Carrying out a serological research method
If we talk about the serological method, it is carried out using kits consisting of 23 bacteriophages, which are divided into four groups. One type of bacteria kills either one or an entire group of phages. Only today this method has lost its popularity because its accuracy is very low and does not make it possible to obtain a complete picture of the disease.
Taking into account the fact that staphylococcus can live in a healthy body, their normal value reaches no more than one hundred pieces. But this does not apply to golden bacteria, because they are considered absolute pathogens and are not normally present in the body. If the diagnosis still reveals a small amount of bacteria in the throat, then the person urgently needs to be treated. The absence of Staphylococcus aureus bacteria in the throat is considered normal.
If the disease was identified in its initial stage, then it will take no more than one week to get rid of its symptoms. To avoid recurrent disease and get rid of purulent plaque, therapy should be continued for another one to two weeks. In the first time after getting rid of the disease, it is necessary to use maintenance therapy, or weak immunity will cause the infection to reoccur.
Treatment of Staphylococcus aureus
The main point in the treatment of staphylococcal infection is antibacterial therapy with drugs to which the pathogen is sensitive. Staphylococcus aureus is one of the few microorganisms that have a high ability to develop resistance to antibiotics.
Microorganisms that “live” in medical institutions are especially dangerous. Over the course of their lives, they have encountered a lot of medications and disinfectants, so it is very difficult for doctors to choose a truly effective treatment for hospital-acquired staphylococcal infections.
Taking antibiotics
Staphylococcus aureus is characterized by increased resistance to many antibacterial drugs. For this reason, antibiotics that are active against this microorganism are used only in the treatment of complicated, life-threatening forms of the disease.
This approach to therapy avoids the development of resistance of certain strains of Staphylococcus aureus to the antibacterial agents used.
Severe staphylococcal infections require the prescription of parenteral (injection) antibiotics, of which preference is given to:
- protected penicillins (Nafcillin, Ampicillin + Sulbactam);
- first or second generation cephalosporins (Cephalexin, Cefuroxime, Cefazolin) in combination with Clindamycin.
Vancomycin is reserved for resistant strains of MRSA; it is also prescribed if the infection is life-threatening.
Immunostimulation
- Autohemotransfusion is the intramuscular injection of a patient’s own venous blood. This procedure is widely used to treat furunculosis.
- Subcutaneous or intramuscular administration of antistaphylococcal antitoxic serum or intravenous administration of antistaphylococcal plasma.
- Herbal immunostimulants - Schisandra, Echinacea, Eleutherococcus, Ginseng, Chitosan. These drugs normalize energy and basal metabolism, have an adaptogenic effect - help cope with stress and stress.
- For patients with severe signs of immune dysfunction, synthetic immunomodulators are indicated - “Polyoxidonium”, “Ismigen”, “Timogen”, “Amiksin”.
The prognosis depends on the localization of the pathological focus of staphylococcal infection, the severity of the disease and the effectiveness of treatment.
With mild lesions of the skin and mucous membranes, the prognosis is almost always favorable. With the development of bacteremia with damage to internal organs, the prognosis sharply worsens, since in more than half of the cases such conditions result in death.
Symptoms of staphylococcus on the skin
IT IS IMPORTANT TO KNOW! A remedy for getting rid of parasites that works immediately. Read more >>>
The symptoms of staphylococcal infection largely depend on the location on the body, the stage of the disease and how the body itself fights bacteria. The microbe is capable of causing many skin pathologies, which have their own characteristic manifestations. What they look like is shown in the photo.
Furunculosis
The formation of purulent boils is a common disease that can cause inflammation of the skin on any part of the body. The most dangerous is the appearance of ulcers on the neck and face. It is here that the infection is located close enough to the brain, where it can also cause an inflammatory process.
How it manifests itself:
- the appearance of small redness with white dots in the middle (accumulation of pus);
- swelling of the inflamed area;
- the appearance of painful sensations (twitching or pulsating attacks in the affected area);
- destruction of the protective film and leakage of purulent fluid outward, formation of ulcers.
Furunculosis - the appearance of ulcers on the body
Prevention
Basic personal prevention measures:
- personal hygiene (clean hands, wet cleaning at least 2 times a week, properly prepared food);
- timely treatment of infectious diseases - dental caries, boils, sore throats, inflammation of the adenoids and tonsils, urethritis and others;
- avoiding crowded places during the peak of respiratory diseases;
- refusal to consume dairy, meat and confectionery products stored improperly, especially in hot weather;
- immediate treatment of skin wounds with antiseptics, applying a bandage or plaster to them;
- refusal to visit beauty salons and dental clinics, which do not pay due attention to the disinfection of medical instruments.
If you experience any skin rashes or feel unwell, be sure to consult a specialist. Staphylococcus aureus has serious consequences for the body and to avoid them, you need competent treatment prescribed by a doctor.