Causes
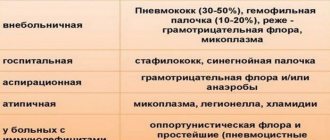
The cause of the development of focal pneumonia can be various infections. In most cases, the causative agents of the disease are bacteria.
It can be:
- Pneumococci;
- Streptococci;
- Staphylococcus;
- Escherichia coli;
- Friedlander's wand.
staphylococcus and streptococcus
Some viruses also cause the disease:
- Influenza virus;
- Parainfluenza virus;
- Adenovirus;
- Rhinovirus.
There are other possible infectious agents:
- Mycoplasmas;
- Proteus;
- Various fungi.
The most common cause of the development of focal pneumonia is pneumococcus.
Factors that provoke the development of the disease in a weakened body predisposed to pneumonia include:
- Chronic lung diseases;
- Hypothermia;
- Smoking;
- Constant contact with toxins that enter the lungs when breathing;
- Stress;
- Depression.
An important provoking factor in the development of focal pneumonia are acute and chronic diseases of various organs of the body in addition to the lungs.
If the patient spends a lot of time lying on his back, the normal functioning of the respiratory organs is disrupted, which can lead to the development of inflammation in them.
https://youtu.be/https://www.youtube.com/watch?v=vZJsHjkjmtg
_
Clinic and symptoms
The clinical picture of this type of pneumonia is characterized by: chills, fever, pain in the chest area.
First, a dry cough appears, which becomes productive as the disease progresses - sputum is released; attention should be paid to its nature in the initial period. Severe shortness of breath - during breathing there is a lag of the chest on the affected side.
The sputum is usually brown, similar to rust.
During the phase in which compactions form, the following potential problems develop:
- increased voice trembling;
- when tapping, the sound is dull;
- lack of listening to vesicular breathing.
Vocal tremors in lobar pneumonia normalize in later stages, with wheezing appearing and breathing first becoming harsh and then vesicular.
The main characteristic symptoms of lobar pneumonia:
- on the affected side, herpetic rashes are possible;
- body position – lying on your back;
- the skin is hot and dry, and the hands and feet are cold;
- the wings of the nose swell when breathing;
- when compactions spread, breathing occurs with the participation of additional muscles.
Forms of focal pneumonia
There are several types of focal pneumonia:
- Finely focal;
- Large focal;
- Focal-confluent.
In small focal pneumonia, the lesions are small in size, which is reflected in the name of this form of the disease.
Accordingly, macrofocal pneumonia suggests the presence of more extensive foci of damage to the lung tissue. They manifest themselves as clearly visible changes on an x-ray, while small-focal changes in the lungs usually cause only a slight change in the pattern of the respiratory organs.
With focal confluent pneumonia, individual foci of inflammation merge. The inflammatory process spreads to several segments of the lung; in particularly severe cases, the entire lobe is affected.
During the examination, the lag of one lung from the other during breathing is clearly diagnosed, the patient develops shortness of breath and cyanosis (blue discoloration of some areas of the skin and mucous membranes).
Based on the location of the disease, two forms of focal pneumonia are distinguished - left-sided - if the inflammation is localized only in the left lung, and right-sided.
Diagnosis of focal pneumonia
Procedures such as:
- general and detailed blood test;
- Analysis of urine;
- sputum analysis;
- fluorography.
The last procedure, which involves obtaining an image of the condition of the lungs, dots all the i’s in defining the disease and distinguishing it from other similar ones.
When listening to wheezing, the patient experiences frequent loose sounds, especially in places of greatest accumulation of microbes (foci of lung lesions).
Tapping the sternum does not change the sounds, making them identical in both bronchitis and bronchopneumonia.
Sputum analysis allows you to clearly identify the genus and group of pathogenic bacteria in order to select the most effective drug to combat them.
Symptoms sometimes coincide with other related diseases, so an accurate diagnosis is determined only after a complete examination.
Symptoms
Chronic focal pneumonia usually develops gradually; the onset of the disease is not acute or pronounced. The appearance of inflammation is preceded by an incubation period, during which the disease does not manifest itself in any way.
After focal pneumonia enters the active stage, characteristic symptoms appear:
- Chest pain appears, which intensifies with deep breaths and coughing;
- Wheezing in the lungs;
- Shortness of breath occurs;
- Breathing and heart rate increase;
- The patient is tormented by a cough - at the beginning of the development of the disease it is dry, then with sputum;
- The nasolabial triangle acquires a bluish tint;
- The sputum is white or yellow and contains an admixture of pus;
- There is pain in the head and back of the head;
- In most cases, body temperature rises - it can range from 37 to 39 ° C;
- Chills appear;
- The patient is concerned about general malaise and weakness.
This is a general picture of focal pneumonia, but this disease has many variants of its course, and its symptoms can be varied. In young patients, the disease can develop acutely, with high fever and chills from the first day.
Cough is the most characteristic sign of focal pneumonia - this symptom manifests itself more often than others. It can have a different character and different intensity.
In the early stages of development, focal pneumonia often resembles bronchitis. In such cases, it is usually diagnosed late, after it has spread to many lobes of lung tissue and cause great harm to health.
Inflammation spreads from top to bottom, gradually affecting the bronchi, bronchioles and alveoli. In some cases, peribronchial foci appear - this is the name given to horizontal areas affected by the disease during the transverse spread of pneumonia.
Lobar pneumonia - symptoms, causes, stages
Symptoms of lobar pneumonia
Lobar pneumonia has an abrupt onset, which includes chills, headaches and chest pain. Symptoms of lobar pneumonia: an increasing cough, which is dry at first, and after 2 days, when the disease begins to enter its second stage, rust-colored sputum appears.
Since the entire pulmonary lobe is excluded from the respiratory process, the patient with lobar pneumonia develops shortness of breath and the temperature rises.
Definition of symptoms of lobar pneumonia:
- the appearance of frequent dry cough;
- fever up to 39-40 degrees, chills;
- pain in the side is severe and intensifies with sneezing and coughing;
- These symptoms are accompanied by shortness of breath, frequent and shallow breathing;
- a characteristic sign of such pneumonia is the appearance of a blush on the cheek on the affected side;
- Herpes appears near the nostrils and on the lips;
- 2-3 days after the onset of the disease, the patient begins to cough up viscous sputum of a brownish-rusty color;
- urine is excreted in small quantities and dark in color. Usually, when analyzed, protein is detected in it;
- the cardiovascular and central nervous systems are often affected;
- appetite disappears, and a brown-white coating appears on the tongue;
- in very severe cases, pulmonary edema develops.
The behavior of a patient with lobar pneumonia changes. He may be excited or, on the contrary, inhibited, delirium may appear, and red spots appear on the face.
This pneumonia should be treated in a hospital setting with antibiotic therapy.
Causes of lobar pneumonia
Lobar pneumonia is caused by pneumococci, which in a healthy person can easily live on the mucous membrane of the upper respiratory tract and oral cavity, but when associated factors appear (decreased immunity, hypothermia), they can cause the disease. Symptoms of lobar pneumonia appear most often in the cold season and affect a significant part of the lung, and sometimes the entire lung.
Typically, the causes of lobar pneumonia are hidden in bacteriological nature, that is, the lungs suffer from bacteria - pneumococci, staphylococci, etc. Together with the air, bacteria enter the body, penetrate through the bronchi into the lungs, linger in the alveoli and lead to the formation of an inflammatory process in them. Exudate appears in the alveoli, which seeps through small blood vessels and is a favorable breeding ground for the reproduction and growth of bacteria. Next, the exudate penetrates through the pores of the alveoli, and inflammation spreads to a significant part of the lung.
Stages of lobar pneumonia
In its development, this pneumonia goes through 4 stages:
1.
At the first stage, the lung tissue turns red, the patency of the capillaries located here is impaired, and the inflammatory process increases. Microorganisms are actively multiplying. This stage of lobar pneumonia lasts up to three days.
2.
Red blood cells and plasma proteins fill the space of the alveoli and small bronchi. The density of the area affected by the disease increases, and its color becomes intensely red. The duration of this stage is from 1 to 3 days.
3.
At the third stage of lobar pneumonia, a large number of neutrophils appear in the alveoli, making them grayish-yellow. The duration of the stage is about 5 days.
4.
And finally, the fourth stage of pneumonia is characterized by the fact that the protein gradually begins to dissolve. When the exudate is completely absorbed, the lung tissues lose their diseased density, but their elasticity, however, is not completely restored. How long this stage lasts depends on the extent of the inflammation, the individual characteristics of the body, the activity of the causative agent of the disease, the chosen course of treatment, etc.
Diagnosis of the disease
When examining patients using instrumental methods, the following are revealed:
- Disturbances in the functioning of the respiratory system, which become noticeable when listening to the lungs - they can manifest themselves as wheezing and hard breathing;
- Disturbances in the functioning of the cardiovascular system: tachycardia, muffled heart sounds, expansion of percussion boundaries;
- Changes in the lungs - each focus of inflammation appears on the X-ray in the form of darkening;
- Changes in the general blood test - leukocytosis or leukopenia, increased ESR.
The most important among all possible examination methods is x-ray. As a rule, the image clearly shows pathological changes in the lung tissues, which are usually concentrated in the lower lobes. This disease differs from tuberculosis.
To differentiate these two diseases, it is necessary to examine sputum for the presence of Mycobacterium tuberculosis.
Diagnosis and treatment
Any suspicion of possible pneumonia should not be ignored, both by the patient and the attending physician. Because this disease, if untimely or improperly treated, can lead to more extensive damage to the lung tissue.
The pathogenesis, etiology and clinical picture of focal pneumonia are varied, but all of them can act as a complication provoked by other diseases or arise independently.
Treatment of focal pneumonia
In most cases, correct, timely treatment can cure the disease, avoiding serious health complications. The basis of treatment is antibacterial drugs.
The most commonly used antibiotics are from the groups of fluoroquinolones, penicillins or cephalosporins. They are administered intravenously, intramuscularly or orally. The optimal duration of treatment with antibacterial drugs is from 10 to 14 days.
As an auxiliary treatment, the following can be used:
- Anti-inflammatory drugs;
- Detoxification therapy;
- Mucolytic and bronchodilator drugs;
- Immunostimulating agents;
- Vitamins to support the body.
Corticosteroids are also used to treat acute pneumonia, which can quickly relieve inflammation.
Drugs in this group include prednisolone and methylprednisolone. Even if treatment helps, positive changes are not immediately noticeable.
On X-ray, the reverse development of changes in the lung tissues becomes noticeable, and the erythrocyte sedimentation rate also gradually decreases, which indicates a decrease in the activity of inflammation.
Complications: what is the danger of focal pneumonia
Focal inflammation of the lungs can cause many disorders in the functioning of the body. All complications of pneumonia are divided into two groups - pulmonary and extrapulmonary.
The first includes acute respiratory failure, which can cause death. When this condition develops, the patient requires artificial ventilation . The most dangerous extrapulmonary complication of the disease is infectious-toxic shock, which can also be fatal.
It is possible to identify characteristic complications for some pathogens.
| Staphylococcus | Pulmonary hemorrhage, pneumothorax, purulent pericarditis, sepsis |
| Streptococcus | Exudative pleurisy and pleural empyema |
| Friedlander's wand | Severe intoxication, increased amount of sputum with copious pus, development of abscesses |
Focal pneumonia in children
In young patients, the inflammatory process is more severe.
When focal pneumonia occurs in children, the following symptoms are identified:
- chills and fever;
- an increase to subfebrile body temperature of the baby, then to critical levels - up to 39 degrees and above;
- deterioration of appetite, general well-being of the child: becomes capricious, whiny, irritable;
- wheezing occurs in the chest, shortness of breath when breathing at rest;
- acquisition of a bluish tone by the skin near the nasolabial triangle;
- increased activity of the sebaceous glands, revealed by heavy sweating;
- dry, obsessive cough with secretion.
This problem in children is always acute and causes serious complications for the baby’s body. If symptoms of the disease are detected, you need to urgently consult a doctor for a diagnosis and treatment.
Prevention
In addition to the heart, inflammation from the lungs can spread to other organs. Focal pneumonia can cause the development of encephalitis, meningitis, and glomerulonephritis.
Vaccination
As with any disease, the risk of developing pneumonia can be minimized by maintaining a healthy lifestyle and following a number of simple measures:
- Dress carefully, avoiding hypothermia;
- Timely vaccination against possible pathogens;
- Take timely measures against bacterial and viral infections of various organs, primarily the respiratory system
- Avoid stress;
- Regularly undergo medical examinations, which allow you to identify the disease in the early stages;
- Eat properly and rationally, making sure that the food contains a sufficiently large amount of vitamins and minerals that are necessary for the normal functioning of the immune system;
- regularly take walks in the fresh air and engage in other physical activity;
- Avoid inhaling aggressive substances, especially for a long time, and carry out wet cleaning of the room in a timely manner.
Since the disease develops gradually and erroneous diagnoses are often made, especially in the early stages of focal pneumonia, everyone should know the symptoms and treatment of this disease.
In this case, the chances of recognizing the disease in time and receiving appropriate therapy are significantly increased, and this allows you to avoid serious complications.
https://youtu.be/https://www.youtube.com/watch?v=E-ArgKbEZr4
_