Pneumonia is a serious disease that affects both adults and children. When a specific microorganism enters the body, mycoplasma pneumonia occurs quickly in children and is often accompanied by influenza and adenovirus infection, which aggravates its course. It is important to know the symptoms that manifest the disease, since early diagnosis and timely treatment are the key to successful recovery.
Causes of mycoplasma pneumonia
Doctors attribute decreased immunity and impaired local defenses to the main causes of pneumonia. The disease is caused by:
- Frequent ARVI, pharyngitis, laryngitis, tracheitis.
- Flu, sore throat, adenoviral infection.
- Reduced immune response in infants and children with concomitant pathologies of internal organs.
- Reduced resistance of the body when taking certain medications (cytostatics, steroid hormones).
- Finding a child in closed groups (kindergarten, boarding school).
The pathogen is transmitted from a sick person to a healthy person by airborne droplets, while the disease develops in a weakened body. After recovery, those who have recovered from mycoplasma pneumonia retain strong immunity. In most cases, the disease does not occur in adults, and re-inflammation is mild.
The development of lung disease in children occurs in several stages:
- Entry of the microorganism into the respiratory tract and fixation on the mucous membranes.
- Active reproduction of bacteria with decreased immunity.
- Dispersal of mycoplasma inside the cells of the mucous membrane.
- Development of clinical symptoms of pneumonia.
In children, pneumonia most often occurs in a mild or moderate form and goes away without a trace, unlike in adults. Women and men with the development of mycoplasma infection are also susceptible to the occurrence of a process in the mucous membranes of the genital organs, which can lead to problems with conception.
Diagnostics
In order for the treatment tactics for Mycoplasma pneumonia in children to be chosen correctly, it is necessary to carry out the required diagnostic procedures. Periodically, the external signs of pneumonia disappear, but this does not mean that the patient’s condition is improving. Treatment tactics will be accurate only when the cause of mycoplasma pneumonia has been accurately established.
There are no specific techniques aimed at detecting this type of pathogen. A complete blood count can help determine if the erythrocyte sedimentation rate (ESR) has increased, but the white blood cell count may remain unchanged. When performing an x-ray, the doctor will see a change in the pulmonary pattern, but it is impossible to see signs that the disease is caused by Mycoplasma pneumoniae. To ensure that the diagnostic results are as reliable as possible, it is recommended to conduct a series of studies.
X-ray examination
From the point of view of the typical picture that can be seen on an x-ray, mycoplasma pneumonia in children will not manifest itself in any way, since the pattern of the lungs is very similar to bronchopneumonia, in which the lower lobe of the lung is affected.
Obtaining an accurate picture is only possible after collecting the patient's medical history. These data will allow the pulmonologist to determine the exact nature of the disease and decide on treatment tactics.
There are only two accurate ways to determine the presence of mycoplasma pneumonia in the body. The described methods are long-term, they take up to 3 weeks - this is a bacterial culture and a blood test for immunoglobulins. These methods are not very suitable for quickly diagnosing bacterial pneumonia.
Bacterial culture
To determine the presence of mycoplasma, it is necessary to obtain a swab from the child’s throat. You can also use sputum secreted during coughing as a material for research. Sowing duration is from 7 to 10 days.
Waiting for a long time for test results is fraught with the development of complications that will begin to show signs in the cardiovascular system, respiratory tract or hematopoietic system. To prevent this situation, specialists prescribe antibiotic treatment to the child. For this purpose, broad-spectrum drugs are selected that are effective against a large number of microorganisms.
Immunoglobulins
This is the name given to proteins that differ in a certain structure.
Their appearance in the body is observed after recent infectious diseases. Immunoglobulins are necessary for the body's systems to prevent the re-development of pathology. If a child shows signs of pneumonia, then it is necessary to take a test that will determine the presence of igg and igm proteins in the blood. The analysis is done twice with an interval of two weeks. The first blood draw is carried out 14 days after the onset of the disease. If the first analysis showed the presence of igg and igm, then this does not completely indicate the development of a form of pneumonia such as mycoplasmosis. The accuracy of the putative diagnosis is guaranteed only if by the end of the fourth week the dynamics of growth in the number of immunoglobulins continues. If the result is positive, then the child has suffered from mycoplasma pneumonia. There is a danger of re-infection, the probability of which is from 7 to 10%.
Manifestations of inflammatory disease
The symptoms of mycoplasma pneumonia are nonspecific and are similar to the clinical signs of other diseases of the respiratory system:
- The increase in body temperature in most cases is insignificant, up to 38 degrees.
- Chills.
- Nasal congestion, runny nose with mucous discharge.
- Paroxysmal, dry cough.
- In older children, cough is accompanied by the production of mucous sputum.
- Pain, sore throat.
- Headache.
- Rarely, a maculopapular rash occurs on the body.
Nonspecific manifestations can confuse parents, who often mistake pneumonia for less dangerous pharyngitis and tracheitis, as well as doctors, who may suspect influenza at the initial stages of diagnosis. To establish an accurate diagnosis of mycoplasma pneumonia, it is important to carefully collect anamnesis, conduct an examination and additional laboratory tests.
Symptoms
Mycoplasma pneumonia in children gives the following symptoms:
- migraine;
- slightly elevated temperature;
- painful to swallow;
- nasal discharge;
- chills;
- dry cough, in which there is pain in the lung on the affected side.
Mycoplasma pneumonia can lead to the development of any inflammation of the respiratory system, such as laryngitis, rhinitis, etc., which further leads to mycoplasma pneumonia. The disease can last for more than one week.
Clinical manifestations are blurred, which is why diagnostic errors occur repeatedly. Typically, this type of pneumonia is confused with the influenza virus. And experienced doctors are convinced that the symptoms and treatment of mycoplasma and chlamydial pneumonia in children are similar.
How is mycoplasma pneumonia diagnosed?
X-ray can detect disease
This pneumonia is difficult to diagnose, since specific changes in it are absent in many laboratory tests.
- A general blood test reveals leukocytosis and acceleration of ESR, which indicates an inflammatory process in the body.
- On auscultation, dry and moist inhomogeneous rales are heard.
- An X-ray of the chest organs reveals an increase in the pulmonary pattern and intense small-focal opacities, localized mainly in the lower parts of the lungs.
- Sputum analysis is nonspecific and only indicates an inflammatory process in the lungs. Isolation of the pathogen is difficult, since mycoplasma is an intracellular microorganism that parasitizes the cells of the mucous membrane of the respiratory tract.
- The main diagnostic method is the serological method, in which specific antibodies to mycoplasma are detected in the patient’s blood serum.
- In acute illness, class M immunoglobulins are detected in the blood, the titer of which increases over 2 weeks, which is a diagnostic criterion for this pneumonia. Only upon recovery do their levels drop to normal.
After recovery and during chronic mycoplasma infection, serological testing is accompanied by an increase in the level of class G immunoglobulins, which provide specific protection. Infants rarely suffer from this form of pneumonia, since during the first six months of life they are provided with immune protection by antibodies that have penetrated the placental barrier.
How does the disease progress?
Typically, the mycoplasma that causes pneumonia enters the body through the respiratory system. The latent period ranges from 1 to 4 weeks. Experiments on volunteers revealed that the disease usually lasts 12-14 days.
The most common first sign of respiratory mycoplasmosis is:
- redness of the back of the throat with enlarged tonsils;
- dry mucous membranes;
- "tickling" in the throat;
- It's difficult to breathe;
- cough without sputum.
In addition to damage to the alveolar and bronchial epithelium, a clear immunomorphological reaction is possible in the lungs.
Mycoplasma entering the body passes through a protective barrier. When it settles on the cells of the ciliated epithelium, a connection between the agent and the immune system occurs, which is characterized by the development of two reactions: the active production of B-cell protein, which causes local antibodyogenesis. In simpler terms, due to the described reaction, immunoglobulins are produced: IgM, IgA, IgG and cellular immunity is triggered. Local immunity that occurs in response to mycoplasma is considered a major component in the development of immunity.
From the first days of the disease, plasma cells appear in the submucosal layer, producing first IgM, and then IgG and IgA antibodies. With mycoplasma pneumonia IgG in a child, antibodies attach to the membrane and are “swallowed” by macrophages. IgA antibodies stimulate phagocytosis of mycoplasmas, they stop the process of settling on the membranes of ciliated epithelial cells, due to which the pathogen does not settle on the mucous membranes, and therefore does not produce substances harmful to the body. In order to activate phagocytosis, in addition to immunoglobulins and complement, the participation of lymphokines will be required. Due to the interaction of the pathogen with antibodies, compliment, and lymphokines, mononuclear and polynuclear leukocytes accumulate and make up the bulk of the exudate that causes inflammation. Mycoplasmas are destroyed in macrophages, their breakdown products, released antigens and biologically active substances, provoke the development of local inflammation with a pronounced immunopathological component. Over time, this reaction becomes more “bright” due to the immune response to substances foreign to the body that are produced in target tissues.
Immune cellular reactions in lesions occur in a slow manner. At this stage in the development of medicine, it became clear that in addition to pneumonia, acute respiratory infections, bronchitis, mycoplasma is similar to non-respiratory diseases, such as Stevens-Jones disease and other systemic diseases. Mycoplasma pneumonia IgM in a child can have both a latent and violent course.
Manifest forms of respiratory mycoplasmosis in children most often lead to changes in the upper respiratory tract (URT). A characteristic symptom of this type of mycoplasmosis is pharyngitis. Inflammations such as rhinitis, sinusitis, otitis media, etc. occur much less frequently.
It should be noted that the symptoms of mycoplasma lesions of the upper respiratory tract have practically no characteristic features and are similar to most other diseases.
How does the infection start?
- The infection begins with an increase in body temperature to 38-39 degrees and general malaise.
- There is a tickling sensation in the throat and a stuffy nose.
- Occasionally there is a runny nose, ear pain, and “dry” eyes.
- The fever goes away in about 2-6 days.
- Inflammation of the oral mucosa is observed within a week, but the release of the pathogen continues for some time.
- If the infection affects the lower respiratory tract, inflammation of the bronchi and lungs occurs.
Scientists have proven that during this period, about 41-62% of all pneumonias are caused by mycoplasmic origin.
The clinical course of mycoplasma pneumonia is similar to an upper respiratory tract infection:
- The febrile temperature persists for a long time.
- Symptoms of “poisoning” of the body are mild, and it is from them that one can suspect mycoplasma pneumonia.
- Among other things, after some time from the onset of the disease, a severe cough occurs that lasts more than a week.
- In older children, cough is usually accompanied by sputum production.
- On auscultation, inhomogeneous dry and variable-sized wet rales are heard.
- X-ray shows bilateral foci of heterogeneous infiltration in the lungs.
- In 11% of children with mycoplasma pneumonia, the disease is accompanied by a maculopopular rash.
Complications of pneumonia
Although mycoplasma pneumonia is mild in the vast majority of cases, in the absence and improper treatment it can be accompanied by serious complications:
- Mycoplasma pleurisy.
- Damage to the nervous system - meningitis, encephalitis, myelitis. Damage to the central nervous system is severe and can leave behind long-term defects.
- Hemolytic complications - autoimmune hemolytic anemia, thrombocytopenia, hemoglobinuria.
- Cardiac manifestations - pericarditis and myocarditis occur very rarely.
- Damage to the skin and mucous membranes - 15% of sick children develop a rash, conjunctivitis, and stomatitis.
- Arthritis.
To avoid serious consequences, it is important to consult a pediatrician in time and carefully follow the treatment prescribed by him.
Prevention
To prevent mycoplasma pneumonia, it is recommended:
- to refuse from bad habits;
- strengthen the immune system;
- eat well;
- sleep 8 hours a day;
- use protective masks during epidemic troubles;
- observe the rules of personal hygiene;
- Don't ignore walks and exercise.
It is necessary to regularly ventilate the premises, as well as maintain optimal temperature and humidity in them.
Treatment of pneumonia
A pediatrician should decipher the analysis and select appropriate therapy; you cannot take medications on your own. Specific therapy for mycoplasma pneumonia should be started immediately. The following are used in treatment:
- Antibiotics - Erythromycin, which is prescribed to children at a dosage of 20-40 mg/kg/day, divided into 3 doses. Clarithromycin and Azithromycin are also used, which are available in the form of suspensions for young children. Treatment with an antibacterial drug continues for less than 14 days. The duration of therapy and dosage are determined by the doctor in each case individually.
- For symptomatic pneumonia, mucolytics and expectorants are used - ACC, Lazolvan.
- Antipyretic drugs - Paracetamol, Nurofen, Nimesulide, are used when body temperature rises above 38 degrees.
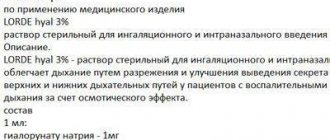
- If your nose is stuffy, you may need saline solutions (Aqua-Maris) and decongestants (Flixonase).
- For itching that accompanies skin rashes, antihistamines (Suprastin) are prescribed.
- If the oral mucosa is affected, rinsing with Stomatidin is indicated.
Treatment of this disease should begin on time and in full. This will speed up the healing process and avoid serious complications.
Basic moments
Mycoplasma is an opportunistic microorganism. It is often found in healthy people, but it can lead to many diseases.
The disease is widespread throughout the world. Both women and men are susceptible to infection. Moreover, mycoplasma pneumonia is more often observed in females. This figure is 40%.
The resource of mycoplasma is infected people, healthy people are carriers of the bacilli. Infection is characterized by seasonal fluctuations and occurs in the late summer and autumn months. Although you can get sick throughout the year.
Children, adolescents, and patients under 35 years of age are most susceptible to infection. These are also people working in societies, school and student associations. Familial cases of infection are possible. Mycoplasma pneumonia is rare in middle-aged and mature adults.
Women who have gynecological diseases, sexually transmitted infections, and have had promiscuous sexual relationships are most prone to mycoplasma.
Types of disease
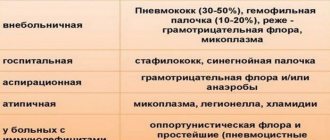
Based on the detected pathogen, there are:
- respiratory mycoplasmosis – the course of this form is characterized by the manifestation of acute respiratory diseases. In critical situations, mycoplasma leads to the development of an atypical form;
- genitourinary form of mycoplasmosis is an infection of the genitourinary system of a venereal nature, which spreads during sexual relations. There is a risk of infection through household methods.
In cases of inflammation of the genitourinary tract, mycoplasmas are detected in 75% of cases. In addition, 10% are healthy people in whom the disease passes without symptoms and does not manifest itself until the body’s protective function weakens.
When the body is subjected to severe stress, during pregnancy, childbirth, abortion, hypothermia, mycoplasma awakens and the disease makes itself felt.
Mycoplasma can cause the following diseases:
- pyelonephritis;
- urethritis;
- arthritis;
- sepsis;
- pathologies of the fetus, pregnancy;
- postpartum endometritis.
Factors
Mycoplasma pneumonia occurs due to infection with this type of bacterium. Every person's body contains them normally. There are situations when aggravation occurs.
One of the development characteristics includes periodic chronization of the algorithm associated with late treatment and generalization of mycoplasma infection. This occurs due to the nuances of the structure of the microorganism, which is similar in structure to human cells. Due to this, protective antibodies are developed late, affecting their own tissues, provoking autoimmune processes in people.
Mycoplasmas can persist for a long period of time in epithelial cells and the lymphopharyngeal ring. They easily pass from a sick, asymptomatic carrier through mucus from the nose and respiratory tract. They are not resistant to external conditions.
- Heating.
- Drying.
- Ultrasound.
They do not grow if the environment is poorly nutritious.
In addition to mycoplasma pneumonia, microorganisms can cause acute inflammation of the respiratory system, exacerbations, and the occurrence of non-respiratory disease in an almost healthy person.
- Pharyngitis.
- Bronchial asthma.
- Chronic obstructive bronchitis.
- Pericarditis.
- Otitis.
- Meningitis.
- Hemolytic anemia.
If mycoplasmosis is not treated, pneumonia will be associated with severe consequences.
Signs of illness
The incubation period for the disease is on average 2 weeks, sometimes longer. The disease caused by mycoplasma develops gradually, although perhaps with an acute, acute manifestation.
The disease spreads with drops of saliva and phlegm released when the patient coughs. Contact infection through objects is also possible.
Initially, the upper respiratory tract is affected, which is typical for catarrhal nasopharyngitis, laryngitis, and rarely the acute form of tracheobronchitis. The patient experiences the following symptoms:
- stuffy nose;
- dry nose;
- sore throat;
- the voice is hoarse.
The state of health noticeably worsens, the temperature gradually increases, the body feels weak, sweat is released.
In the case of acute manifestations of poisoning, signs appear on the first days of inflammation. If the development is gradual, for 7-12 days.
The disease initially causes a long, dry cough. During an attack, it is quite strong and tiring. A small amount of viscous mucus and pus are released, and sometimes there are traces of blood. The cough can become chronic and persist for 4-6 weeks due to resistance to the respiratory tract and significant activity of the bronchi.
By the 7th day of illness, the symptoms increase. The temperature reaches 40 degrees and does not subside all week. The cough is severe, pain is felt in the chest while breathing. During the examination, the specialist reveals fine bubbling rales, a shortened sound during percussion, and focal weakness of vesicular breathing.
Mycoplasma pneumonia may include symptoms of interstitial lung inflammation.
When the disease occurs outside the pulmonary course, the following symptoms develop:
- rash on the skin, eardrums;
- myalgia;
- feeling of discomfort in the gastrointestinal tract;
- sleep is disturbed;
- not a severe headache;
- paresthesia.
It is also possible that fibrinous or exudative pleurisy may occur, and pleuritic pain may occur.
If the case is not complicated, the signs of mycoplasma pneumonia gradually disappear within 10 days. There is a threat of the disease becoming a mixed form due to the addition of a secondary pathogen.
A blood test shows the absence of leukocytosis, increased ESR.
The course of the disease is most often good, but sometimes complications occur.
- Meningitis.
- Arthritis.
- Nephritis.
Disease prevention
Pneumonia is easier to prevent than to treat an advanced infectious process. To prevent mycoplasma pneumonia, it is necessary to:
- Take antibacterial drugs prescribed by your doctor for at least 2 weeks in order to achieve a complete recovery and prevent relapse of the disease.
- During the period of convalescence, perform exercise therapy, massage, and breathing exercises with the child (you can inflate balloons).
- After recovery from mycoplasma pneumonia, sanatorium-resort treatment is indicated in cities with a warm, dry climate.
- It is important to take a preventative course of multivitamins (Vitrum, Alphabet).
- It is necessary to harden the child and engage in general strengthening of his body (walking in the fresh air, swimming, physical exercise).
- In the autumn-winter period and during epidemics, it is recommended to avoid crowded places and visiting closed groups (kindergartens, boarding schools).
- It is important to be vaccinated according to the schedule if there are no contraindications to vaccination.
For children who are often and long-term ill, who are more at risk of developing mycoplasma pneumonia, dispensary observation is established, which helps to identify the symptoms of a dangerous disease in a timely manner and prescribe appropriate treatment.
Although the symptoms of this disease are not specific, you cannot ignore them or self-medicate. Timely contact with a specialist and careful implementation of medical prescriptions are a guarantee of successful recovery.
Author of the publication: Irina Ananchenko
Remember! Self-medication can cause irreparable consequences for your health! At the first symptoms of the disease, we recommend immediately contacting a specialist!
Causes
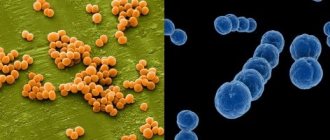
Pneumonia develops as a result of the penetration of pathogenic strains of single-celled organisms of the genus Mycoplasma into the respiratory tract. Mycoplasma pneumoniae is a prokaryotic anaerobe that does not have a cell membrane.
Microorganisms attack membranes or penetrate into target cells (epithelial cells of the bronchial and tracheal mucosa, epithelium of the walls of the pulmonary alveoli and red blood cells).
After mycoplasma penetrates the cellular structure, the body attacks the infected cells, provoking the occurrence of autoimmune processes. Reactions underlie the symptoms of the disease.
Causes of the disease
Mycoplasmas become the causative agents of pneumonia very often. Microorganisms do not live long in a dry air environment, exposed to ultraviolet solar radiation, but many of them manage to penetrate the human body before dying.
- The infection is transmitted through the air. When a sick person coughs or sneezes, pathogenic bacteria fly out of his mouth along with saliva and sputum particles, spread through the air, and settle on furniture and household items.
- A healthy person only needs to inhale contaminated air or touch an infected item before eating to become ill. Therefore, people with pneumonia should always cover their mouths with a handkerchief or at least their palm when coughing and sneezing.
And healthy people should not forget to wash their hands with soap before eating.
Due to poor hygiene, children suffer from mycoplasma pneumonia more often than adults. The incubation period of the disease reaches four weeks. In most cases, the initial stage of the pathology does not manifest itself acutely. Inflammation of the lungs caused by mycoplasmas can be of three types according to the characteristics of their manifestation:
- respiratory;
- non-respiratory;
- generalized.
Treatment
All patients with mycoplasma pneumonia are given etiotropic antibacterial treatment, choosing drugs to which the microbe is most sensitive.
Typically, antibiotics from the group of tetracyclines are used - "Tetracycline", "Doxycycline", macrolides - "Azithromycin", "Erythromycin", fluoroquinolones - "Ciprofloxacin", "Ofloxacin". The course of treatment is 21 days. Acute pneumonia is treated in a hospital. Patients are prescribed bed rest, diet therapy and adequate drinking up to two liters per day. Fruit drinks, water, juices, compotes, and rosehip infusion are especially useful for patients.
Symptomatic treatment:
- Expectorant drugs – “Ambrobene”, “Bromhexine”, “ACC”,
- Antipyretics - Ibuprofen, Paracetamol,
- Analgesics – “Analgin”, “Baralgin”,
- Immunomodulators – “Imunorix”, “Ismigen”,
- Throat sprays – “Inhalipt”, “Tantum Verde”, “Cameton”.
In case of severe respiratory manifestations, protracted course of the disease and low effectiveness of conventional methods of administering antibiotics, the aerosol method of administering drugs has a good effect. It gives especially good results when combining antibiotics with proteolytic enzymes - chemotrypsin and lidase. These enzymes facilitate access of the drug directly to the site of inflammation, help to liquefy bronchial secretions and clear the airways of it. If pneumonia is mild, the use of symptomatic and restorative agents is sufficient.
Auxiliary methods that allow patients to rehabilitate faster are: exercise therapy, hydrotherapy, physiotherapy, massage, sanatorium and resort treatment.
Folk remedies that increase the effectiveness of drug therapy and speed up the healing process - infusion of St. John's wort, chamomile, cornflower, blackberry, inhalation with pine needles and eucalyptus.
The criteria for recovery may be fluoroscopy data, as well as indicators of specific and nonspecific immunity.
Treatment methods
Treatment of mycoplasma pneumonia is prescribed exclusively by the attending physician. Attempts to treat yourself are extremely dangerous for the patient’s health and can result in serious complications.
As a rule, treatment of pulmonary mycoplasmosis is complex in nature. According to medical prescriptions, the following are often prescribed:
- antibiotics;
- mucolytics;
- antitussive drugs.
Antibiotics are designed to directly combat the causative agent of the disease. Based on the results of laboratory tests, doctors often prescribe antibiotics belonging to the classes of macrolides, tetracyclines, fluoroquinolones and others. Depending on the specific medicine, they can have both a bactericidal (destroy) and bacteriostatic effect (prevents them from multiplying) on the causative agents of mycoplasma pneumonia.
Remember that antibiotic treatment is always associated with a large number of side effects for the patient’s health. This is another reason to entrust the choice of medicine to a specialist.
Mucolytics or expectorants are prescribed to improve sputum discharge in the patient.
Antitussives are often prescribed at the very beginning of mycoplasma pneumonia. Their task is to relieve pain when coughing.