A little physiology
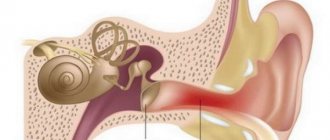
The functionality of the middle ear is to conduct sound by transferring wave-like air vibrations collected by the auricle into the cavity of the inner ear.
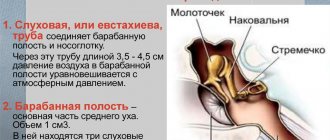
The middle ear is located in the temporal bone, and air from the nasopharynx enters here through the Eustachian tube.
The external auditory canal and the cavity of the inner ear are separated by a thin, translucent membrane, which is familiar to everyone as the eardrum.
During the development of any disease that is accompanied by a runny nose, in some cases, mucus from the nasal passage through the Eustachian tube enters the middle ear cavity. This is called otitis media, and in some cases, eardrum bypass cannot be avoided. Also, this disease can begin to develop against the background of adenoiditis.
Pathogenic microorganisms that enter the middle ear cavity along with mucus begin to multiply rapidly. As a result, an acute form of otitis media develops. After some time, an accumulation of lymphoid tissue occurs in such a confined space - this is purulent otitis media.
In the language of medical professionals, pus is called exudate. An excess of this mass leads to severe pain. The lack of proper and timely treatment ends with the puncture of the eardrum in order to remove the purulent mass.
Like any other surgical intervention, the eardrum bypass procedure also has certain indications for its implementation. In this case, a significant reason is the presence of purulent masses in the ear cavity, which cannot be treated conservatively.
Direct indications for tympanostomy include the following pathological conditions:
- An acute form of otitis media, in which there is no pronounced pain syndrome, and the eardrum itself is not damaged.
- Purulent form of otitis media against the background of perforation, when it is not possible to administer medicine and remove purulent masses.
- Development of otitis media with the formation of exudate.
- Sensorineural hearing loss.
- Narrowing of the Eustachian tube.
- Barotrauma of the ear.
In addition, there are other, no less serious cases:
- Ear inflammation occurs frequently, and drug treatment is not effective.
- Decreased hearing quality due to constant accumulation of fluid in the middle ear cavity.
- Balance imbalance.
- Decreased auditory functionality, causing a delay in speech development.
- The patency of the Eustachian tube is impaired.
In addition, eardrum bypass in adults or children is also performed for the purpose of diagnosing diseases that are difficult to detect in any other way. In this case, tympanostomy is the only option to detect pathology in a timely manner.
How is the bypass procedure performed?
An incision on the eardrum is made with a special, reduced surgical scalpel under the control of a microscope. A shunt is then inserted into the incision and secured. The operation itself will take no more than 30 minutes and is quite easily tolerated by both adults and children.
The procedure for bypassing the tympanic cavity requires mandatory anesthesia, which is associated with a high concentration of nerve endings on the membrane connecting the middle ear to the ear canal.
The type of anesthesia is selected by the doctor based on the patient’s age and individual characteristics:
| Patient's age | Type of anesthesia for bypass surgery |
| Over 18 years old | Local anesthesia (in the absence of relevant contraindications) |
| Children under 8 years old | General mask anesthesia |
| Children from 9 to 18 years old | General or local anesthesia (the choice depends on the child’s behavior, since the operation requires complete immobility of the patient) |
Attention! After installation of a shunt, the patient may experience hearing loss and the appearance of extraneous noise. These symptoms are not dangerous and disappear on their own after the tube is removed and the membrane heals.
When the patient is completely cured, the shunt is removed by an otolaryngologist, and the hole in the membrane heals on its own. If this does not happen, the surgeon uses a special allograft to close it.
Possible complications
Most eardrum bypass operations go without any problems, only occasionally the following complications occur:
- re-infection of the middle ear cavity (most often occurs when water gets in), which occurs in 99% of cases if the patient behaves incorrectly;
- prolonged non-healing of the hole in the eardrum after removal of the shunt, requiring plastic surgery;
- scar formation (in most cases does not lead to changes in hearing);
- repeated inflammation of the middle ear (usually milder and responds well to conservative treatment);
- early loss of the shunt from the ear (can lead to relapse and require repeat shunting).
Fortunately, all possible complications, if identified in a timely manner, can be quickly corrected.
Rehabilitation period
After bypass surgery under general anesthesia, the patient remains in the hospital under the supervision of the attending physician (stay time depends on the age and general condition of the patient).
If local anesthesia is performed and there are no complications, the patient can go home within 3-4 hours after surgery. Further monitoring of the progress of recovery is carried out on an outpatient basis.
Before discharge, a consultation with a doctor is required, who will describe in detail all the recommendations for a speedy recovery and indicate the nearest date for examining the patient at the outpatient clinic.
What should you do at home after surgery?
- The main requirement is to protect the sore ear from water (especially liquids from the pool or natural bodies of water). When taking a shower or bath, the patient is recommended to protect the ear canal with a special plug or a homemade cotton swab lightly dipped in oil.
- It is forbidden to sneeze and cough while covering your nose and mouth (there is a danger of the tube falling out).
- Instill drops with antibacterial properties, prescribed by a doctor, into the auricle.
- In case of severe pain, take painkillers (these will also be prescribed by the doctor).
At the Konstanta Clinic in Yaroslavl, eardrum bypass in children is performed by experienced ENT doctors of the highest category.
Find out how much the bypass procedure costs at the Constanta Clinic in Yaroslavl by making an appointment with a specialist by phone: (4852) 37-00-85 Daily from 8:00 to 20:00
Sign up for a consultation
The approximate cost of bypass surgery in children, as well as prices for additional Clinic services are listed here.
What is ear shunting
If the above methods do not help and the health condition worsens, ear bypass surgery is prescribed.
Ear bypass surgery is a surgical procedure using special optical instruments. Its essence consists of a micro-incision in the eardrum, through which a small and narrow plastic tube is inserted. Air passes through it into the drum area, maintaining pressure.
In a healthy human body, this procedure is carried out by the auditory tube, but at the time of illness the procedure is very problematic. Since during the course of the disease the tube narrows in size, the passage of air is impossible.
Usually shunts are made of plastic, but in case of individual intolerance they are made of metal or Teflon.
There are two types of shunts:
- For limited time use;
- For long-term wearing.
Short term tubes should be used for no more than one year. However, the distinctive feature of this element is that the shunts fall out on their own.
Shunts for long-term wear are larger in size and are fixed in the ears with specialized stoppers. The shunt is removed with the help of a doctor.
It is noted that this operation is performed on people who frequently fly on airplanes. Due to changes in pressure in the ears, a feeling of fullness occurs. In order to avoid this, shunts are introduced.
Another case of shunt insertion is damage to the eardrum.
Typically, eardrum bypass occurs when there is pus in the ear, which has not responded to drug treatment for a long time.
Rehabilitation period
After surgery, it is advisable for the patient to remain in the hospital for 2-3 days. If there are no complications, the patient is discharged and can go home. After the procedure, the patient should not feel severe discomfort or pain at the incision site. Some people experience slight pain in the ear during the recovery period; this is considered normal for 2-3 days after surgery.
After anesthesia, the patient may feel dizzy and nauseous, so bed rest is recommended. People after surgery sometimes experience irritability and aggressiveness, which arise immediately and pass just as quickly. As a result of the manipulation, hearing is completely restored in almost 90% of patients.
Some people complain that all the surrounding sounds are very loud. In this case, the doctor prescribes appropriate sedative medications. To avoid bacteria and infection entering the tympanic cavity, the organ should be protected from moisture and water. The duration of the postoperative period varies from 7 days to 1 month, depending on the person’s immune system and compliance with all the specialist’s recommendations.
Eardrum bypass in childhood
Ear bypass surgery in children is usually performed between the ages of one and three years. Since this age group is most characterized by the manifestation of purulent otitis media and other pathological conditions of the ears.
Due to the physiological characteristics of the structure of the Eustachian tube, children, more often than adults, need specialized medical care aimed at normalizing the pressure and outflow of fluid from the ear.
Otolaryngological surgery (tympanic membrane bypass) is performed in young patients under general anesthesia, which allows the head to be fixed in the desired position.
In case of purulent or exudative otitis media, surgical intervention is limited to a small incision of the eardrum, which allows for the removal of fluid accumulated in the ear cavity.
In case of chronic pathological processes in the ear, an incision is not limited to; installation of a special shunt is required.
Eardrum bypass in children is performed using small-diameter temporary tubes to properly handle fluid removal and ventilation.
If necessary, a medical specialist instills antibacterial drugs into the sore ear to promote healing of the mucous surface of the ear.
Using ear drops for a speedy recovery
Indications for ear bypass surgery in children
Otitis, or inflammatory diseases of the ear, is classified according to the location of the inflammation into external, middle and internal. When a small patient comes in with complaints, a pediatric otolaryngologist prescribes a comprehensive treatment, including taking antibiotics, anti-inflammatory drugs, performing physical procedures, as well as introducing proteolytic enzymes and mucolytics into the ear. If the treatment did not bring the expected relief, shunting of the eardrum of the child’s ear is prescribed if the following pathological processes are detected:
- regular occurrence of inflammation of the middle ear (more than once a year);
- hearing loss;
- dysfunction of the vestibular apparatus;
- the appearance of speech problems;
- congenital obstruction of the eustachian tube.
Paracentesis
Due to the increased density of the eardrum in children and the associated pronounced pain syndrome during exudative otitis media and the pre-perforative stage of purulent otitis media, in some cases an incision of the eardrum is made without installing a shunt (paracentesis). This allows you to remove pus and quickly relieve pain.
In most cases, installation of a shunt is not required; inflammation of the hearing aid can be successfully treated with conservative methods.
If the outcome of the disease is favorable, the child’s incision will heal on its own within 1-2 weeks.
Indications for surgery
Surgical intervention is indicated if a person experiences inflammation in the tympanic cavity several times a year, which cannot be completely cured with antibiotics and other medications. Manipulation is prescribed if the patient’s hearing progressively decreases, chronic accumulation of fluid in the middle ear is diagnosed, and the functioning of the balance organ is disrupted.
Shunting is indicated for:
- hearing loss, which negatively affects a person’s speech;
- pathological changes and congenital anomalies that impair the patency of the auditory tube;
- narrowing of the auditory tube;
- risk of tympanic cavity rupture due to pressure fluctuations;
- barotrauma that occurred during diving or airplane flights;
- mechanical injury to the middle ear.
If the patient is diagnosed with exudative otitis media, then this is a direct indication for shunting. The manipulation allows you to free the eardrum from accumulated fluid and normalize the functioning of the hearing organ. It is advisable to perform surgery if conservative treatment is ineffective: ventilation, catheterization, and use of medications. In this disease, the shunt is installed for 2 to 3 months.
Possible consequences and complications
Complications after eardrum bypass are rare. These include:
- Mild pain.
- Painful intensification of auditory sensations.
- Disorientation in space.
- Post-drug effects – irritability, moodiness.
- Illusion of tinnitus, hearing impairment. They disappear after removal of the shunt and fusion of the eardrum.
Against the background of reduced immunity, inflammatory reactions may develop, which can be stopped with drugs such as Dexon, Garazon, etc. An exacerbation of bacterial infections cannot be ruled out. In such cases, antibacterial ear drops are used - Otofa, Tsipromed.
Alternative to tympanic cavity bypass
An alternative method for treating middle ear diseases is paracentesis. A distinctive feature of the procedure is that after the doctor makes an incision in the tympanic cavity, a tube is not inserted into it, and the exudate is removed through the incision.
An alternative manipulation is most often performed in children with exudative inflammation or purulent otitis media. Surgery helps remove fluid from the ear cavity through an incision, which closes itself within 1-2 weeks. Installation of a shunt is not required, since after removal of purulent formations, further treatment is carried out with the help of medications and conservative therapy.
Manipulation reduces ear pain and alleviates the patient’s general condition. If paracentesis does not have positive results, the patient needs to undergo bypass surgery. If there is persistent dysfunction of the ear canal, middle ear surgery should be performed to eliminate the underlying cause of the disease.
Surgical intervention, both bypass and paracentesis, is performed on patients of any age. After a detailed examination by a doctor, reviewing the patient’s medical record and receiving test results, the specialist prescribes a comprehensive and most appropriate treatment for the disease.
Therapy using a shunt in the tympanic cavity is very effective, since it reduces the risk of inflammatory processes in the hearing organ, reduces excessive accumulation of exudate, minimizes the likelihood of scars and adhesions in the ear cavity, partially or completely restores hearing, improves speech, eliminates imbalances. Many patients note that after the procedure, sleep normalizes and pain in the ears ceases to bother them.
What complications can there be?
If the treatment regimen and hygiene rules are violated in the postoperative period, specific complications may arise due to infection. In this case, a strong inflammatory process will develop in the middle part of the ear.
For reasons beyond the control of the surgeon and the patient, the following complications very rarely occur:
- Scarring of the eardrum, in which connective tissue grows around the shunt and protrudes inward, impairing the functionality of the auditory ossicles;
- perforation of the membrane along the incision line and loss of the shunt;
- premature loss of the tube, in which the shunt does not have time to perform its functions, and the membrane is tightened.
In the latter case, patients are advised to have a repeat operation, and in the first two cases, if the functionality of the eardrum is impaired, its plastic surgery is recommended. But such complications are very rare; as a rule, the recovery process is easy for patients.
The eardrum bypass procedure is used by otolaryngologists around the world to eliminate hearing problems and treat ear diseases. It is performed quite simply, and its safety has been proven by many years of experience of doctors and patients. If a person suffers from chronic otitis, shunting can significantly alleviate his condition and speed up recovery. It is necessary to consider its features and implementation methodology in more detail.
Contraindications
In general, the tympanostomy procedure has virtually no contraindications and is safe for humans. However, there are some cases when it is better not to carry out such an operation:
- Neoplasm in the middle ear cavity (neurinoma, meningioma).
- Abnormal development of the vascular system - the internal carotid artery passes through the cavity of the middle ear.
- Slowing down blood clotting.
Also, this procedure is contraindicated in cases where it is impossible to conduct a visual inspection of the eardrum.
Features of tympanic cavity shunting
An ear shunt is installed surgically. This intervention is called tympanostomy or myringotomy. This procedure requires making a small hole in the eardrum.
The operation has one difficulty. When installing an ear shunt, the child must keep his head still. That is why small children are given light mask anesthesia, during which they sleep.
For adults and older children, general anesthesia is used. During surgery, a myringomy is initially performed, and after that, if there is fluid in the middle ear, it is aspirated. The next step is to install an ear shunt into the hole.
After surgery, some surgeons prescribe ear drops. The patient uses them for several days.
In the absence of complications, surgery is performed within 20 minutes.
If patients have adenoids, then adenoma is performed along with shunting. When performing such an operation, the risk of recurrence of purulent otitis media is significantly reduced.
How you feel after surgery and possible complications
After the operation, the patient remains in the hospital for several days. If he has no complications, he is discharged. During the postoperative period, the patient does not feel pain. Some patients experience a slight sensation of pain in the ear area during the postoperative period.
After surgery, hearing is restored in absolutely all patients. Some patients feel that the sounds are very loud for them. In such cases, the doctor prescribes special medications.
To prevent bacteria from entering the middle ear, it is necessary to protect the ear when swimming in the postoperative period.
This procedure is used by otolaryngologists around the world. This is explained by its absolute safety of surgical intervention.
In some cases, complications may arise in the form of:
- Perforation of membrane
- Infections
- Scarring
- Premature shunt failure
More information about ear shunting can be found in the video.
If the shunt falls out prematurely, there is a risk of recurrence of otitis media. In this case, the operation is often repeated. In some cases, otitis in adults and children occurs after surgery.
This operation can be performed at any age.
If the eardrum is not closed after the shunt falls out, perforation of the eardrum may occur. In this case, plastic surgery of the eardrum is performed.
Ear shunting is an absolutely safe surgical intervention that is aimed at improving hearing that has been lost as a result of frequent purulent otitis media.
Noticed a mistake? Select it and press Ctrl Enter to let us know.
Currently, surgeons use 2 types of shunts:
- A smooth shunt is installed in the eardrum for a certain period of time. After it has performed its function, a specialist can remove it. Modern shunts, as a rule, do not require any removal measures - they fall out on their own as the eardrum tightens. The process of membrane overgrowth takes from six months to a year.
- A shunt with a flange is inserted into the eardrum for several years, and is held in place for a long time due to the sides on both edges of the cylindrical tube. Such a device is installed for irreparable dysfunction of the Eustachian tube, as well as for administering medications in the treatment of sensorineural hearing loss. This shunt has a much wider hole diameter than its temporary counterpart.
Postoperative period
After completion of the eardrum bypass operation, the patient remains within the walls of the medical institution for several days. If there are no complications or deterioration in health, the child is discharged. In most cases, a person does not notice painful manifestations of the ear after the operation.
Some patients complain of nausea, mild pain, and irritability, characteristic of the effects of anesthesia, which disappear in a short time.
All patients experienced complete restoration of hearing function after otolaryngological surgery. Some people experience too much hearing sensation, which is easily corrected with medication.
The recovery period after eardrum bypass involves following a number of recommendations for caring for the operated area of the ear:
- Avoid swimming in pools and natural bodies of water.
- Avoid direct contact of ears with water. When bathing, you need to cover your ear with cotton wool soaked in oil.
- When sneezing or blowing your nose, do not cover your mouth and nose. You should blow your nose by pinching each nostril alternately, with minimal effort.
- Regular visits to the doctor are necessary to monitor the condition of the ear cavity.
Tactics of drug treatment in the postoperative period
An employee of a medical institution prescribes specialized medications based on the patient’s health condition and age characteristics. During the recovery period after ear shunting, the otolaryngologist, in most cases, prescribes a course of anti-inflammatory and antibacterial drugs:
- “Tsipromed”, “Otofa” - drops of targeted antibacterial action;
- “Dexon”, “Anauran”, “Garazon”, “Sofradex” - are effective against inflammation and bacterial cells;
- “Otipax”, “Otinum”, “Normax” - anti-inflammatory ear drops;
- Vitamin complexes that stimulate the immune system promote rapid recovery.
| Drugs | Photo | Price |
| Tsipromed | From 134 rub. | |
| Anauran | From 285 rub. | |
| Otipax | From 306 rub. | |
| Otinum | From 226 rub. | |
| Normax | From 146 rub. |
Treatment with folk remedies
Unconventional methods in restoring the functions of the auditory tube after shunting are used only after consultation with a qualified doctor, since independent choice of traditional medicine recipes can lead to serious consequences for a small organism. The most harmless and effective means include:
- An infusion of two teaspoons of crushed bay leaf and a glass of boiling water is kept for three hours. The liquid is used to rinse the ears.
- Crushed aloe and Kalanchoe leaves are wrapped in gauze and inserted into the ear canals overnight.
- Calamus root boiled in a glass of water, take a tablespoon before each meal. The decoction effectively restores hearing.
- A teaspoon of marsh geranium is diluted in a glass of water. After an hour, the infusion is ready for use. Take 16 g three times a day.
- A tampon soaked in glycerin and wormwood is used as a compress on the sore area.
- Propolis with oil is used as a compress. You need to mix two parts olive oil with one part alcohol propolis.
- A clean and dry geranium leaf is kneaded with your fingers and placed in the ear canal.
The main rule when performing procedures is compliance with hygiene standards. If unpleasant symptoms, painful sensations in the ear, or allergic reactions occur, you must abandon the chosen method immediately.
How can one suspect that a child has exudative otitis media?
The very manifestation of this disease is hearing loss. But it often happens that parents regard the appearance of this disease as a feature of the child’s character, as the child’s whims. The fact that the child does not want to hear them, he is capricious, he asks again or ignores what he is told.
It may appear that the child has restless sleep, watching television programs and cartoons at increased volume. This may even manifest itself in the fact that the child may lag behind in speech and mental development.
The middle ear is connected to the external environment through the internal auditory tube, also called the Eustachian tube. The Eustachian tube opens in the posterior parts of the nose and nasopharynx. The function of this tube is that it is involved in ventilation and equalization of pressure in the middle ear, as well as the outflow of mucus from the middle ear.
Often in children, middle ear disease is caused by dysfunction of this auditory tube. And the cause of this dysfunction is often adenoid vegetation of the nasopharynx in children.
Possible complications
Surgery is used to treat people all over the world. The operation is performed by an otolaryngologist or surgeon. The manipulation is considered absolutely safe and extremely effective. Sometimes patients experience complications: infectious processes in the middle ear, scarring (does not lead to hearing impairment), adhesions, premature loss of the tube (due to this, the inflammatory process in the organ may worsen and re-installation of the shunt will be required), perforation of the tympanic cavity (sometimes required plastic surgery on the tympanic cavity).
It occasionally happens that after the tube is removed, the hole in the middle ear does not heal, in which case a minor additional operation is necessary. The doctor sews up the hole with threads that dissolve on their own.