In what cases are antibiotics prescribed?
With tracheitis, viruses can infect the lower respiratory tract. In this case, sputum appears with purulent discharge and high temperature.
If such signs are observed, the doctor may prescribe strong medications. In this case we are talking about antibiotics. Such substances can help prevent the development of the most serious diseases.
To prevent complications, bactericidal substances are used:
- When there is a possibility of pneumonia;
- The patient has been suffering from a cold for a long time (symptoms persist for more than 30 days);
- Elevated body temperature for several days (this criterion can indicate the severity of the disease and an increased threat of the formation of dangerous complications);
- Symptoms of otitis in acute form;
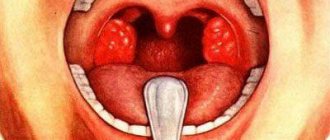
- Sore throat with pus.
Today, doctors prescribe antibiotics with extreme caution. Moreover, not all doctors leave positive reviews about the drugs.
This point of view is proven by the fact that the use of antibacterial substances in the normal course of tracheitis causes harm to the body. Antibiotics contribute to the destruction of normal microflora of the gastrointestinal tract.
After using such drugs, in any case, it is necessary to restore the functioning of the digestive system.
Also, treatment of common tracheitis with antibiotics helps harmful microorganisms adapt to them. In a similar way, when complex ailments of the respiratory system appear, most of the substances may turn out to be absolutely powerless in the fight against viruses.
https://youtu.be/https://www.youtube.com/watch?v=gKkdyd7THto
_
What antibiotics treat tracheitis?
When prescribing an antibacterial drug, the patient's age and symptoms are taken into account. To prevent the growth and further activity of microbes, the doctor prescribes medications with a wide range of effects.
An antibiotic for tracheobronchitis should act not only on the upper passages, but also on the lower parts of the respiratory canal.
In childhood, greater preference is given to penicillins. They are safe, have a minimum of contraindications and side effects. Adults are recommended to take tablets from the group of macrolides or fluoroquinols. If antibiotics are prescribed for tracheitis, the list will include new generation drugs to which bacteria are not resistant.
Penicillin group
This category of drugs is considered one of the most frequently prescribed. Natural remedies include:
- Penicillin;
- Bicillin;
- Benzylpenicillin.
These drugs are sold in the form of powders for making solutions. But in most cases they are powerless, since bacteria have developed a strong immunity to them. Therefore, semi-synthetic medications are prescribed in the form of tablets, capsules and suspensions.
When tracheitis develops, antibiotics from the penicillin group are prescribed to both adults and children from birth.
This group of medicines includes:
- Amoxiclav. Quickly and effectively copes with all types of gram-positive and gram-negative bacteria. The bactericidal and bacteriostatic effect is due to the presence of amoxicillin and clavulanic acid in the composition;
- Amoxicillin. The active component is semi-synthetic penicillin. Has a wide range of effects. But some bacteria are resistant to it. Often prescribed to adults and adolescents;
- Augmentin. Structural analogue of Amoxiclav. The drug is active against many gram-positive, gram-negative, aerobic and anaerobic bacteria. Destroys even those microbes that produce beta-lactamase, which makes the medicine effective for any disease;
- Flemoxin Solutab. The medication is available in the form of tablets, which, when interacting with water, dissolve and form a suspension. Contains amoxicillin. It has a wide range of effects. Prescribed for children over one year of age and adults.
Penicillins are well tolerated by patients, but cannot always overcome bacteria. With frequent use, microbes develop resistance. The duration of treatment averages from 7 to 10 days. If there is no effect within three days, then it is necessary to replace it with other drugs.
Macrolides
In the absence of a positive result from drugs from the penicillin group, macrolides are used as a replacement. They act much faster. The effect is enhanced several times, as the active substances accumulate in tissue structures and affect the body for several more days.
Macrolides are not toxic, so they are prescribed to babies from three months. At the same time, they destroy all gram-positive bacteria, aerobes and atypical microbes.
This category of medicines includes:
- Sumamed. The active ingredient is azithromycin. One pack contains only three tablets, and this is enough for three days of use. Available in the form of tablets and suspensions;
- Azithromycin for tracheitis. Cheap analogue of Sumamed;
- Erythromycin. Representative of the macrolide group. The active ingredient is erythromycin. Most often prescribed to patients in childhood.
Treatment with representatives of the macrolide group is 3 days for mild illness. In case of a complicated form of the disease, an antibiotic is taken for 5 days.
Cephalosporins
When a patient has an adverse reaction or there is no effect on antibiotics of the penicillin group, cephalosporins are replaced. These drugs are used as injections for giving injections.
There are several generations of antibiotics:
- 1st generation. They are prescribed if tracheitis is caused by streptococcal infection. This category of drugs includes Cefazolin, Cefalotin, Cephalexin;
- 2nd generation. Used to treat adolescents and adults. In childhood they can have a strong toxic effect;
- 3rd generation. They are considered the most effective drugs from the entire group. Not only tracheitis is treated, but also complications. Prescribed for young children and adults. This group includes Suprax, Pancef, Cefixime, Ceftriaxone for tracheitis;
- 4th generation. Serious medications are prescribed only if the disease is severe. These include Ladef, Cefepim, Maxipim.
If tracheitis occurs in women during pregnancy, cephalosporins are not used, as they have a negative effect on the fetus. In such cases, Vilprafen or Klacid will come to the rescue. These are representatives of the macrolide group.
When injections are difficult for patients to tolerate, the doctor may prescribe Ciprofloxacin. This medication belongs to fluoroquinols. It is quickly absorbed by the body and begins to act in just a few hours.
Fluoroquinols
Such antibacterial agents have a wide range of effects and effectively cope with many bacteria. They are recommended for use if microbes are resistant to penicillin. Often prescribed for staphylococcal infections, pneumonia and bronchitis in adults.
Fluoroquinols are instantly distributed throughout all tissues, and therefore act on the body for a long time. But they have an adverse effect on the intestinal flora. This group of medications includes:
- Tsiprolet;
- Ciprofloxacin;
- Avelox;
- Moximac.
They are not prescribed to children and pregnant women, as the drugs have an adverse effect on the musculoskeletal system.
Features of application
Doctors often prescribe antibiotics not only for adults, but also for children. For the treatment of children, drugs must be prescribed with great caution.
These are too powerful remedies, so you must adhere to several rules throughout the entire course of treatment:
- It is necessary to take and discontinue medicine for tracheitis only as prescribed by the doctor.
- Carefully observe the dose and time of administration.
- Take medications with exclusively clean water, unless the instructions provide other advice.
- The first dose of the substance for tracheitis should be started with the lowest dose to exclude allergies.
- If secondary results occur, be sure to inform your doctor, but do not stop taking the antibiotic yourself.
- Treatment with antibiotics for tracheitis should be a full course. Otherwise, the surviving bacteria will show stability to the drug and will not produce results with further treatment with the same drug.
- With tracheitis, you need to drink a lot of fluid so that all harmful substances are quickly eliminated from the body.
- You need to understand what medications an antibiotic can be combined with for tracheitis, even if you are taking herbs. Thus, you can avoid the undesirable consequences of treating tracheitis with antibiotics.
- Eat right, and the main food product during the period of taking antibiotics for tracheitis should be fermented milk products in order to restore the functioning of the gastrointestinal tract.
- After completing the course of treatment for tracheitis, be sure to give the baby probiotics to restore the microflora of the intestinal tract.
In some cases, for tracheitis, especially in serious forms of the disease, it is better to use antibiotics as injections.
They are often prescribed for infants, since the damage to the body is less than other forms of drug release. Despite the fact that the child is afraid of injections, if the injection therapy is prescribed, such treatment is still mandatory.
Although all children are afraid of injections, when the doctor directly advises a similar form of therapy for tracheitis, there is no need to refuse it for no reason.
Rules of antibiotic therapy for tracheitis
The first rule of taking antibiotics is that they can only be prescribed by a qualified doctor. Only he is able to qualitatively assess the need to use a particular drug in a specific situation. Self-medication with antibiotics often leads to the development of various side effects and complications. Often patients incorrectly choose the dose of the drug they need, which sometimes provokes an overdose.
In addition, you need to follow the correct regimen for taking the antibacterial agent, which depends on its pharmacological properties. Some drugs (penicillins) must be taken strictly on an “empty stomach”, others (clarithromycin) can be taken with food. You cannot independently adjust the dosage of the drug or discontinue it, even if the patient’s health has significantly improved.
It is best to take antibiotics at a fixed time of day. To take a capsule or tablet of medication, it is recommended to use plain water. Weak tea or still table water are also allowed. This is due to the fact that some components that are included in drinks can affect the absorption of antibiotics and other drugs. Therefore, it is forbidden to drink antibacterial agents with alcohol, coffee, juices, carbonated drinks and dairy products.
If you miss taking an antibiotic, do not panic. It is enough just to take the missed dose of the drug as quickly as possible and continue therapy as usual. At your next doctor's appointment, you need to report what happened.
If the patient notices side effects, he should immediately contact his doctor.
Only he must decide whether it is necessary to cancel therapy, replace the drug, or whether the patient’s anxiety is unreasonable and he needs to be reassured and given psychological support.
Signs of tracheitis
Symptoms of acute tracheitis are expressed after the formation of inflammation of the upper respiratory tract.
The most common criterion for the disease is dry coughing, mainly at night, and also in the morning.
Also, with tracheitis, coughing attacks are observed when taking a deep breath, when laughing, or even when there are changes in air temperature in the room.
During such unpleasant symptoms, especially when the patient has coughing attacks, there may be pain in the throat and chest area. And with an insignificant concentration of sputum during tracheitis, attacks of powerful spasmodic cough occur.
With concomitant laryngitis, there may be a hoarse voice. The general condition of the patient, as a rule, is not characterized by any significant complications.
The temperature is slightly elevated, but only in the late afternoon. In children, it may not exceed 39 degrees.
Sputum with tracheitis is initially viscous with an admixture of mucus, however, after a couple of days. More often this is a period of 4 days and the sputum is removed much easier, but with an admixture of pus.
Since the elimination process is facilitated, it becomes easier to breathe, and the pain is a little less.
There are cases when, together with the trachea, the bronchi are affected as a result of the inflammatory process (with bronchitis) and the picture changes significantly.
In this case, the disease takes on the name tracheobronchitis. With tracheobronchitis, the cough becomes constant and the body temperature is higher. The formation of bronchitis with pneumonia (pneumonia in combination with bronchitis) is especially risky.
In any case, the diseases are quite serious, so at the slightest symptoms you need to immediately consult a doctor and not self-medicate.
As for the causes of tracheitis and the differences between the disease in adults and children, they are the same. There is only one difference, which relates to the methods of treating the disease.
If we consider diseases from the point of view of the fact that the baby’s body is not yet fully formed, then it is much easier to prescribe the drug to an adult.
Not all antibiotics can be taken by children, especially for children, so a doctor can always tell you how to choose a medicine. The drug should be eliminated from the body as quickly as possible. So, the medicine will not harm the little patient.
Treatment of tracheitis must be carried out under the supervision of a doctor.
The main goal of the physician and father and mother when curing tracheitis in children is to increase immunity and saturate the body with vitamins.
The main symptom of chronic tracheitis is paroxysmal coughing.
Other signs of tracheitis:
- Burning sensation in the chest area and lethargy;
- Headache;
- Labored breathing;
- Compression of the ribs when breathing;
- Sore throat and loss of voice.
When is it appropriate to use antibiotics?
Is tracheitis treated with antibiotics? For bacterial tracheitis, systemic and local antibiotics can be used.
Antibacterial drugs are effective only against bacterial flora. They are used if the disease is of bacterial or bacterial-viral origin.
For viral and fungal tracheitis, antibiotics are not used.
To determine the etiology of the infectious process, a number of laboratory tests are carried out.
A detailed blood test helps determine whether tracheitis is infectious or allergic, and bacteriological studies (culture of a smear from the trachea and sputum) identify infectious agents and their sensitivity to a certain type of antibacterial drugs.
It must be borne in mind that the doctor will receive the first information about the presence of bacteria, which a tracheal smear analysis can provide, in 7-14 days, therefore, for the treatment of bacterial tracheitis, broad-spectrum antibacterial agents are prescribed.
Groups of antibiotics and doctors' reviews of the best drugs
Before prescribing an antibiotic, the doctor conducts a full examination of the patient and, based on the data obtained, prescribes a medicine (age, health, temperature, stage of the disease).
Doctors are of the opinion that substances of the penicillin category, which are administered parenterally, are considered effective remedies for tracheitis. In first place is the drug Augmentin.
Antibiotics are available in tablet, suspension or powder form.
Taking antibiotics for pregnant women is extremely harmful. When a patient has significant sensitivity to the components of the drug, the doctor can determine the drug category of cephalosporins.
The best substance in this category is considered to be the antibiotic Cephalexin .
In some cases, macrolides are used to treat tracheitis. These substances are non-toxic and act instantly. In addition, macrolides settle in the matter of the respiratory organs, so their effect is better.
Doctors consider Azithromycin to be the best macrolide. The antibiotic is available in the form of pills, powder, and capsules. Vilprafen can be taken by children over 14 years of age, as well as pregnant women.
The doctor will definitely tell you how many days to take the medicine.
Therapy in pregnant women
Speaking about therapy in pregnant women, it should be noted that treatment should begin immediately after the first negative symptoms form. This will minimize the process of damage to the female body, as well as the fetus. An important condition for starting the recovery process should be the use of medications that are only permissible for pregnant women.
They are characterized by a milder therapeutic effect, to achieve which you can start using the products with minimal dosages. It should be noted that:
- we are talking about such medicines as Berodual, Bioparox, Erespal, Pulmicort, Amoxicillin;
- in addition, if a woman gives birth for the second or more times (accordingly, her body is prepared for drug effects to a much greater extent), it is permissible to use ACC, Lazolvan, Sumamed, Ascorin, Amoxicillin, syrup;
- if there are certain chronic and other diseases in the medical history, it is necessary to use such remedies that are sometimes used for children, such as Ambrobene, Biseptol, Ascoril and other remedies that significantly speed up the overall process, making it, moreover, less associated with complications that arise on their own.
It is advisable to purchase such medications for tracheitis exclusively in pharmacies and only after they have been approved by a specialist. This makes it possible to count on their high degree of effectiveness, as well as on the fact that the recovery will be optimal in duration - for adjustment you can take Berodual or Pulmicort, ACC, Sumamed, Amoxicillin.
Alternative cures without antibiotics
For a serious form of throat disease and complications, no better remedy than an antibiotic has been invented. However, when the disease is mild, traditional medicine can be used as an additional treatment.
Alternatively, the disease can be treated without antibiotics. In this case, you need to pay attention to the temperature, which should not exceed 38 degrees.
Decoctions of eucalyptus and St. John's wort have demonstrated antibacterial properties. A decoction of chamomile and calendula has an anti-inflammatory effect for tracheitis.
Herbs are used as a mouth and throat rinse. You can also select several plants from the listed herbs and inhale them.
Children under the age of one year are prohibited from inhalation, so as not to cause suffocation.
List of antibiotics in the table:
| Drug name | Dosage | A course of treatment |
| Amoxicillin | The usual antibiotic dosage for adults and children is 500 mg 3 times a day. Children under 2 years old – 20 mg/kg body weight/day. | up to 12 days |
| Azithromycin | For adults and children over 12 years of age, the antibiotic is prescribed 500 mg/day at a time. | 5 days |
| Amoxiclav | In case of severe respiratory tract infections - 1 tablet. (500 mg+125 mg) every 8 hours. | up to 14 days |
| Augmentin | For adults and children over 12 years of age, the antibiotic is recommended 1 tablet 3 times a day. For severe infection, a single dose is 1 tablet of 0.625 g. | Up to two weeks |
| Vilprafen | Adults and children over 14 years old - 1-2 g/day. | The duration is determined by the doctor |
| Biseptol | Children 2 - 5 years old: 240 mg of antibiotic 2 times. in a day; from 6 months — 2 years, 480 mg. For adults and children over 12 years old, 960 mg 2 times. | up to 2 weeks |
| Suprax | Dosage for children over 12 years of age and adults 400 mg. | no more than a week |
| Ampicillin | Orally 0.25 g of antibiotic 4 times a day | from 5-10 days |
| Ciprofloxacin | 250 mg, and in more severe cases 500 mg 2 times a day | from 7-10 days |
| Ceftriaxone | Adults and children over 12 years old - 1-2 g 1 time per day | The duration of the course depends on the severity of the disease. |
| Macropen | Up to 5 kg child - 3.75 ml of mixture. Adults: 400 mg 3 times. | 10 days |
| Rulid | 150 mg of antibiotic orally with an interval of 12 hours. Children (body weight over 40 kg) are prescribed 150 mg orally. | The doctor determines the duration after the tests |
Recommendations for taking an antibiotic
Antibiotics should only be prescribed by a doctor after examining the patient and taking tests. A bacterial infection can also be detected by a specific plaque. But independent use of antibacterial drugs can lead to a deterioration in the general condition. Based on age, the doctor prescribes certain medications and their dosage. Before taking it, you should read the instructions and make sure there are no contraindications. Do not change the dose or discontinue the medicine if there is significant improvement. This can lead to resistance and even greater activity of the bacteria.
Doctors also highlight several rules:
- Tablets or suspension should be taken at regular intervals. In this way, the maximum concentration of the active substance is achieved in the blood.
- Take the medication with a small amount of water.
- During antibiotic therapy, adhere to a strict diet. Eliminate spicy, fried and smoked foods, alcoholic and carbonated drinks, and sweets from your diet. This will relieve the digestive tract and avoid side effects.
- If the effect of the medicine is absent within two to three days, then you need to consult a doctor again. The doctor will replace the medicine with another or adjust the dosage.
- You should take probiotics while taking antibiotics. They will maintain the balance of beneficial microflora and increase the body’s immunity, thereby healing will come much faster.
Treatment of tracheitis should be comprehensive. Anti-inflammatory drugs, drugs for gargling, inhalation, gargling and drinking plenty of fluids are added to antibiotics. With proper treatment, recovery occurs within 7-10 days in the absence of complications.
How to take antibiotics correctly?
For antibiotics to have maximum effect, it is necessary:
- Do not interrupt the prescribed therapeutic course.
- Maintain a constant concentration of antibiotics in the blood by observing the frequency of their administration, strictly ensuring that the same time intervals are maintained between the use of the medicine.
- Carefully monitor the therapeutic effect of the antibacterial agent taken. The absence of any improvement in the patient’s condition within seventy-two hours after starting the use of the antibiotic indicates that the bacteria are resistant to medications of this group and a replacement of the drug is required.
Read further: Medicines that support intestinal microflora when taking antibiotics